Though self-harm is not a mental health disorder, it is often a symptom of other conditions, which makes understanding self-harm facts and statistics essential.
Self-harm involves a person damaging their body by cutting, burning, scratching or practicing any other behavior that results in pain or injury. Different motivators can encourage people toward self-harm, such as feeling overwhelmed or numb. Though self-harm is not a mental health disorder, it is a common symptom of many psychological conditions. Self-harm statistics and facts show the widespread trend of self-harm throughout the United States.
Article at a Glance:
- Self-harming behaviors include cutting, burning, and scratching oneself.
- The rates of self-harming behaviors are likely much higher than the statistics actually reported.
- Teens have the highest rates of self-harming behaviors.
- Self-harming behaviors are often co-occurring with eating disorders and substance abuse.
- Self-harm is not a mental health condition in itself, but treatment is available if self-harm is connected to drug and alcohol abuse.
Self-Injury Prevalence
Even though self-harm has been studied extensively for over a decade, findings are never entirely accurate because of the stigma and shame that still surrounds self-injury. The actual rates are likely quite higher than those currently reported.
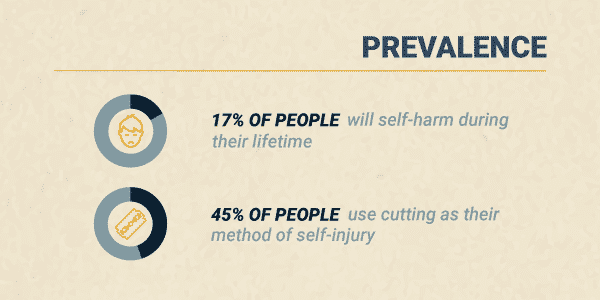
One analysis of self-injury across more than 40 countries found that:
- About 17% of all people will self-harm during their lifetime
- The average age of the first incident of self-harm is 13
- 45% of people use cutting as their method of self-injury
- About 50% of people seek help for their self-harm but only from friends instead of professionals
Not only is self-harm prevalent, but rates are increasing. According to emergency room trends, there’s been a 50% increase in reported self-injury among young females since 2009.
Who Self-Harms?
While anyone can practice self-harm, rates tend to differ among certain populations:
- Adults. Aside from very young children, adults are the least likely group of people to follow through with self-injury. Only about 5% of adults have self-injured in their lifetime.
- Teens. Adolescents have the highest rate of self-injurious behaviors, with about 17% admitting to self-injury at least once in their life.
- College Students. Studies find that about 15% of college students report engaging in self-harm.
- Women vs. Men. While women are more likely to self-harm, males may represent at least 35% of total self-injury cases. Men are more likely to underreport self-injury and have other people hurt them than women.
- Sexual Minorities. Gay and bisexual people are at a high risk of self-injury. Nearly half of all bisexual females engage in self-injury.
Age of Onset
As mentioned, the average age of onset for self-injury is 13. This age seems to align with new stressors and expectations at school and home as the child enters their teenage years. Age 13 represents a time of great physical, social and mental change and development. This time is also linked to the emergence of mental health conditions like anxiety and depression, which may further trigger a desire to self-harm.
Related Topic: How long does depression last?
Self-Harm Risk Factors
There is not just one factor that contributes to self-harm. Instead, there are a variety of biological and environmental issues known to cause self-harm, including:
- Having friends or family members who self-injure
- Experiencing stressful life situations like traumatic events, family instability and sexual identity uncertainty
- Living in social isolation
- Mental health conditions, like depression, anxiety and personality disorders
- Drug and alcohol use or addiction
The more of these factors a person has, the higher their risk of self-harm.
Diagnosing Nonsuicidal Self-Injury Disorder (NSSID)
Nonsuicidal self-injury is not a diagnosable mental health condition: yet. Currently, the American Psychiatric Association (APA) lists nonsuicidal self-injury as one of the “Conditions for Further Study” in the most recent Diagnostic and Statistical Manual of Mental Disorders (DSM-5). This designation implies the group may include the condition in future versions of the text.
Nonsuicidal self-injury involves symptoms like:
- Engaging in self-harm on five or more days over the last year
- Self-injuring to find relief from an unwanted feeling, solve a relationship conflict or create a desired feeling
- Self-harm involves unwanted feeling like depression, anxiety or anger, an intense focus on completing the behavior and frequent thoughts of self-injury
Since self-injury is not currently an official mental health diagnosis, a medical or mental health professional will ask the person questions about the behavior and the purpose of the behavior to assess the situation.
Rates of Self-Harm and Co-Occurring Conditions
Self-harm often co-occurs with mental health disorders. Historically, self-harm was thought to be directly connected to borderline personality disorder. Now, it’s understood that the behavior can be associated with many conditions, like:
One study found that of people who self-injure:
- 20% have personality disorders
- 13.5% have adjustment disorders
- 11% have mood disorders, like depression or bipolar disorder
Addition research shows that about 55% of people who self-harm have eating disorders.
Although the conditions may overlap, nonsuicidal self-injury is often not linked to:
- Obsessive-compulsive disorder (OCD)
- Excoriation (skin-picking) disorder
- Trichotillomania (hair-pulling disorder)
Self-Harm and Suicide
Although an act of self-harm is different from a suicide attempt, there is a strong association between self-injury and suicide attempts. It seems that as incidents of self-harm increase, the likelihood of suicide attempts also increase.
People who engaged in 20 or more self-harm behaviors are about 3.5 times more likely to attempt suicide compared to those who have fewer self-injury actions.
Self-Harm Prognosis
Establishing a self-harm prognosis is based on:
- Frequency of self-harm
- Intensity of self-harm
- Duration of self-harm
- Presence of other mental health symptoms or conditions
- Available professional or social support
The APA reports in the DSM-5 that self-injury tends to peak by the time a person is 29, so the prognosis improves as age increases.
Statistics on Self-Harm Treatment
Since self-harm is not a mental health condition of its own, tracking treatment statistics is challenging. What experts do know is that treatment must focus on the factors that trigger self-harm, as well as the self-harm itself.
For example, if your self-harm is connected to substance use, getting help from The Recovery Village could reduce self-harm as you find recovery from alcohol and other drugs. Call today to speak to a representative about available treatment options for self-harm and substance use disorders.
Related Topic: Finding Support for Addiction & Mental Health with Teletherapy
Are you or a loved one struggling with self-harm, suicidal ideations, or other dangerous self-destructive behaviors? The Nobu app is great tool to learn more about mental health topics and connect with mental health professionals. It is free and for anyone that is looking to reduce anxiety, work through depression, build self-esteem, get aftercare following treatment, attend teletherapy sessions and so much more. Download the Nobu app today!


The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
