Heroin withdrawal is a necessary undertaking when addressing heroin addiction. However, there are options available to detox in a safe and comfortable way.
To recover fromheroin addiction, one must first go through the process of ridding the body of heroin and its toxic metabolites. The process is known as detoxification or, more commonly, “detox.” As the body clears the heroin out, the unpleasant experience ofdrug withdrawaloccurs.
For many people with addictions, the fear of withdrawal is a major barrier to escaping their addiction. For some people, that fear keeps them from even trying addiction treatment. However, millions of people have successfully found health and happiness in long-term recovery.
Fortunately, withdrawal and detox don’t have to be a terrible experience. By participating in an inpatient detox and withdrawal program, people can get through the experience safely and comfortably.
https://www.therecoveryvillage.com/wp-admin/post.php?post=13832&action=edit
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
Article at a Glance:
- After initially stopping heroin, terrible flu-like symptoms arecommon, such as runny nose and muscle aches.
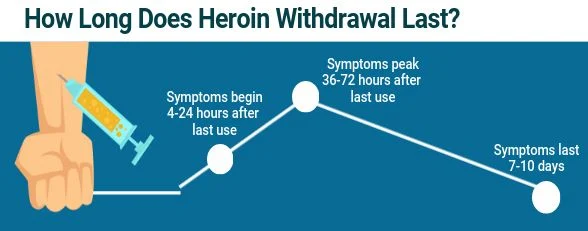
- The symptoms of withdrawal from heroin typically start within the first four to 24 hours and peak within 36 to 72 hours.
- Heroin withdrawal symptoms can last for seven to 10 days.
- It is not recommended to quit heroin “cold turkey” or detox at homebecause many home remedies for heroin detox are unsafe, untested, and unproven.
- Amedical facility is the safest and most effective place to detox.
How Long Does Heroin Withdrawal Last?
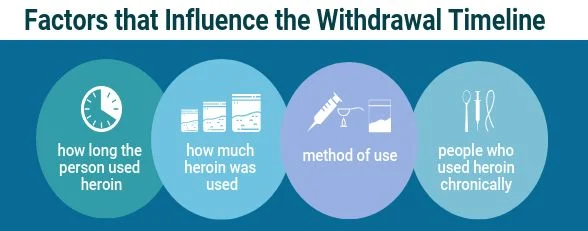
Different opioid drugs havedifferent timelinesfor withdrawal, and it depends on how much and for how long the individual used heroin.
For heroin, the withdrawal symptoms start within the first 24 hours (sometimes as soon as four hours) from the last use, peak within 36 to 72 hours, and last seven to 10 days for most people. People who use heroin chronically may experience some withdrawal for up to three or four weeks.
When Does Heroin Withdrawal Start?
For heroin,the withdrawal symptoms startwithin the first 24 hours (sometimes as soon as four hours) from the last use, peak within 36 to 72 hours, and last seven to 10 days for most people. The severity and duration of withdrawal may depend on how long the individual used heroin, as well as the amount and method of heroin use. People who use heroin chronically may experience some withdrawal for up to three or four weeks. While withdrawal is a necessary undertaking when addressing heroin addiction, there are options available to detox in a safe and comfortable way.
How Long Does Heroin Stay in Your System?
When heroin enters the body, it is rapidly metabolized. This happens so quickly that most of the drug is out of the system within 30 minutes. Thehalf-life of heroinis about three minutes. For example, if someone injects 20 mg of heroin, then 10 mg is left after three minutes, 5 mg after six minutes, etc. Heroin will be completely clear from the body in about 15 minutes for many people, but some people metabolize heroin more slowly. In this case, heroin can stay in the system for 30 minutes or longer. Drug tests can measure heroin in saliva, blood, urine, and hair for different lengths of time.
How Do You Taper Off of Heroin?
Atapering regimenis all about lessening tolerance and dependence over time. Taking less and less of the drug allows the body and nervous system to self-correct and, ultimately, heal itself. By keeping withdrawal symptoms at bay, it is more likely that an individual will continue the recovery process. This is one of the primary reasons replacement therapy is used as well. A person’s environment will play a vital role in deciding how to taper off heroin.
Is Quitting Heroin Cold Turkey a Good Idea?
Quitting cold-turkey is not recommended as it is the most difficult and dangerous way to attempt to address addiction.Medically-supervised detoxwith withdrawal medications, counseling support, and symptom management make the experience much easier, safer and more likely to result in a successful recovery.

Stopping heroin “cold-turkey” brings about a rapid onset of withdrawal symptoms, which are very difficult to endure. The risk ofexperiencing a setbackduring withdrawal is high as the craving to use and stop the symptoms can be overwhelming. When people try to self-taper their heroin use on their own they are seldom successful. A relapse during withdrawal sometimes leads tooverdose.
Heroin Withdrawal Medications
Opioid replacement therapy involves a long-acting opioid medication that is used to keep drug cravings and withdrawal symptoms to a minimum without causing a high. Over time, the dose ofthese drugs can be taperedin a slow and controlled manner until the patient is opioid-free.
Only two opioids areFDA-approved for the treatment of heroin withdrawal: methadone and buprenorphine. Buprenorphine generally has a more favorable side-effect profile than methadone. One type of buprenorphine product used during opioid detox isSuboxone, which also contains naloxone, which blocks opioid receptor sites to prevent any attempts at abuse.
Other medications may also be used during heroin detox to help with specific symptoms. These include sedatives (such as benzodiazepines) and the medication clonidine, which helps reduce some withdrawal symptoms.
Abouthalf of peoplewith addictions also suffer from mental health disorders, such as depression or anxiety. Recognizing and treating underlyingmental health disordersprovides the best success rates for recovery and is an important part of returning the person to good health and functioning.
Heroin Withdrawal Deaths
Withdrawing from heroin is typically safer than withdrawing from alcohol, but it isoccasionally fatal. When people die from heroin withdrawal, it’s usually due to excessive vomiting and diarrhea. Untreated, these symptoms can rapidly dehydrate the body and cause dangerously high levels of sodium to accumulate in the blood (hypernatremia) and the heart can fail. Such cases occur when people withdraw from heroin on their own, usually in jail. Such deaths can be prevented by medical supervision in a professional detox facility.
Heroin Withdrawal Tips
The primary tip for heroin withdrawal is not to do it alone. Withdrawal is a difficult experience and willpower alone is seldom adequate to prevent relapse. There is plenty of help out there to make detox and withdrawal safe and less uncomfortable. Utilizing the supports in place is the best way to get on track for long-term recovery. A specialized treatment facility with medically-assisted detox is the safest method for quitting heroin and avoiding relapse.
Heroin Detox
Professional heroin detox is medically-supervised withdrawal from heroin. Detox must be done as part of an overall plan for recovery, which involves much more than simply stopping using the drug. The underlying causes of the addiction and the mental devastation from the addiction itself must be addressed for the best chance of successful recovery and a return to good health and happiness. Detox for a serious addiction like heroin is almost always an inpatient process.
For some people, likely for those whose heroin use was limited,outpatient detoxtherapy may be an option. Even though their use of heroin was not severe enough to warrantinpatient treatment, they are still psychologically susceptible to using it again. As such, they will be required to attend meetings andcounseling sessions.
Aninpatient heroin detox programis a natural transition to counseling, which forms a crucial part of the overall treatment plan. Arecent studyshowed that inpatient detox is the most effective way to ensure a successful recovery after discharge.
Other Methods for Detox
Helping Someone Withdrawing or Detoxing From Heroin
It’s best to talk to an addiction specialist team to obtain advice before helping a loved one through the detox and withdrawal process. Addiction specialists are trained in how to work with people in withdrawal. They can offer expert support with the task of helping a loved one through the withdrawal process. To talk to a specialist,call us, or sign up for online counseling services throughThe Recovery Village Telethealth App.
Before withdrawal and detox begin, it’s important toclear all drugs and drugparaphernalia out of the house to avoid tempting the individual.
It can be very stressful to watch someone go through heroin withdrawal. Although heroin withdrawal is seldom deadly, stopping heroin can lead to very uncomfortable symptoms within only a few hours. Besides the physical symptoms, the person withdrawing may show psychological symptoms, such as confusion, anxiety, and aggression.
Because recovery is a lifelong process, the individual will require ongoing support. The person in recovery will need a strong support system after detox completes. This support system may include long-term professional counseling sessions. Some counseling sessions may be available tofriends and familyas well.
Therapy After Detox
Regardless of the merits of acute heroin detox versus outpatient heroin detox, neither approach will be very successful without the presence of counseling following the actual detox process.As mentioned earlier, a heroin addiction devastates both the mind and the body. Detox addresses the damage done to the body; counseling addresses the mind.
Finding a Heroin Withdrawal & Detox Center
The do-it-yourself detox methods are not worth the risks and can lead to far more damaging effects on the body. Undergoing detox at a professional facility is a safe and effective way to rid the body of drugs like heroin.








