Detoxification cleanses the body of drugs and alcohol. Learn what to expect during drug or alcohol detox and where to find reliable detox resources.
Drugdetox treatmentis the first step in overcoming a drug or alcohol use disorder. Substance and alcohol use can change a person’s brain, making it hard for them to function normally without using the substance or alcohol. Drug detoxification is the process where a person is weaned off of a drug so that it is no longer in their system.
Top Takeaways:
- Drug detox is the first critical step in overcoming addiction, involving the process of allowing the body to eliminate toxins from drug use under medical supervision to manage withdrawal symptoms safely.
- Detox programs vary and can include inpatient, outpatient, and medical detox options, each tailored to the individual’s specific needs and the severity of their addiction.
- Drug Detox can be a critical step toward recovery. Our evidence-based approach combines medical support and counselling to promote lasting change. The Recovery Village serves individuals across the United States with compassion and expertise.
- Medical supervision during detox is essential to monitor vital signs, manage withdrawal symptoms, and provide support to ensure a safe and effective detox process.
- Withdrawal symptoms can range from mild to severe, depending on the substance and duration of use. Medical professionals can administer medications to alleviate symptoms and provide emotional support during this challenging phase.
- Detox is just the beginning of the recovery journey. Comprehensive treatment plans, including therapy, counseling, and aftercare programs, are crucial for maintaining long-term sobriety and addressing the underlying causes of addiction.
- Each individual requires a personalized detox plan based on their unique medical history, type of substance used, and overall health to ensure the most effective and safe detox experience.
- Having a strong support system, including family, friends, and professional counselors, is vital in helping individuals stay motivated and committed to their recovery journey.

Drug and alcohol medical detox programs aid people who want to overcome their substance use disorder, safely and effectively. Detoxification, especially when guided by medical professionals through analcohol medical detox program, is the first step toward recovery from any substance use disorder.
What Is Drug Detox?
The definition of detox is the process of abstaining from alcohol or drug use until the bloodstream is clear of the substance. In other words, drug detox involves ridding an individual’s body of the substance it has come to depend on to feel normal. During this process, the person may experience withdrawal symptoms.
Drugs That Cause Withdrawal
There are many substances that can alter the brain and the way a person feels. These substances can become addictive. When used in excess and a person relies on them to feel normal, stopping their use can cause withdrawal symptoms. Drugs that cause withdrawal include:
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.

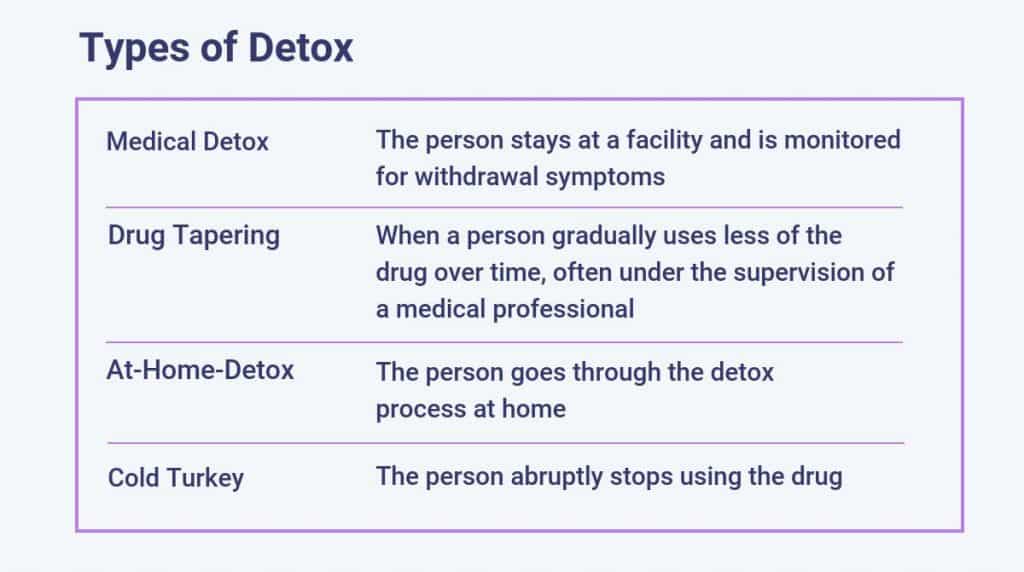
Types of Drug Detox
There are many different ways that a person can detox from a drug. Most detox methods are difficult to endure, as the person will most likely experience unpleasant, and sometimes serious, withdrawal symptoms. It’s always a good idea to have the supervision of a medical professional when detoxing.
What to Expect During Detox
It’s important to understandwhat to expect during detoxbefore going to rehab. The detoxification process can take anywhere from days to weeks, as a person’s body adjusts to life without the substance. During this process, a person may undergo a series of side effects and withdrawal symptoms that can be mild or severe. The following factors are descriptions of what medical detox is like.
The Dangers of Improper Detox
A person with a substance use disorder may have serious withdrawal effects if they try to quit too abruptly or on their own. The dangers of detox can range from physical symptoms to psychological symptoms. If a person experiences severe psychological symptoms, it could lead them to want to harm themselves. It is usually better to work with a medical professional to develop a drug detox plan and have supervision during the process.

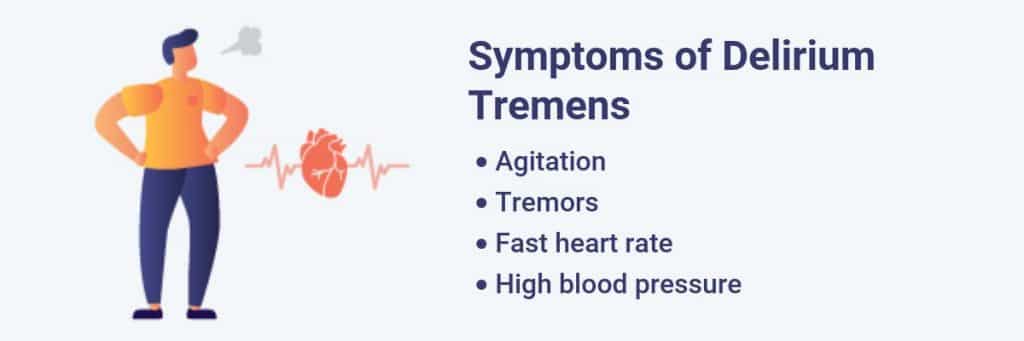
There are dangers of detoxing at home without the supervision of medical professionals. One serious withdrawal effect of alcohol use isdelirium tremens, where a person may experience agitation, tremors, a fast heart rate and high blood pressure. This effect usually occurs within 24–48 hours after stopping alcohol use. It can be deadly, with amortality rate of 37%when it is not treated.
How Long Does Detox Last?
How long drug detox takes depends on the substance used, the amount of the substance used and the length of time the person has been using the substance. It can also depend on the person’s physical and mental state when they start detox. People who are highly motivated to begin the medical detox process may be able to handle the symptoms better than people who are reluctant to quit.
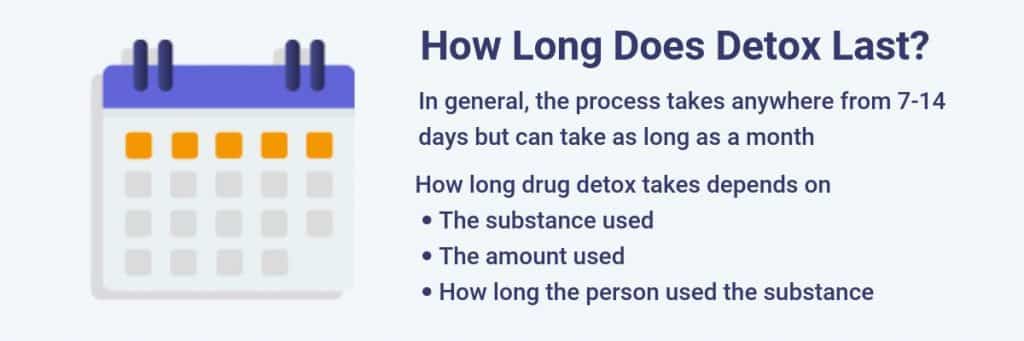
If a person is using more than one substance or has a co-occurring mental health issue, the detox process could take longer. In general, the process takes anywhere from seven to 14 days but can take as long as a month.
Next Steps After Detox
Detox is the first step in overcoming a substance use disorder and living a healthier life. After completing detox, it can be difficult to maintain this lifestyle and not return to the old habits of substance use. To continue to recover after detox, a person will usually undergo additional therapy to address underlying conditions or reasons that may have caused them to use in the first place, likeinpatient treatment.
Inpatient treatment programs allow the person to receive rehab in a setting that is free from temptations and distractions. The medical team will develop an individualized treatment plan that will help the person overcome the physical and psychological effects of their substance use disorder. The plan will generally involve therapy and medication when appropriate.
Inpatient treatment can be followed by residential treatment where the person lives in a community where they can receive more long-term care for their substance use disorder. These programs usually last for six months or more.
Detox Programs Near Me
The Recovery Village has comprehensive detox programs that are tailored to each client’s unique physical and psychological needs. Each of our medical detox programs are medically supervised, offer 24-hour clinical support and mental healthcounseling, and provide a transition to further rehab programming.

Insurance May Cover The Cost of Detox
Your insurance plan may cover some or all of the cost of medical detox. Our online health insurance verification system will estimate your in-network and out-of-network deductibles, coinsurance percentages and out-of-pocket maximums. Within 5 minutes, you’ll receive an email with these details – free of charge. Fill out the form below to get started:








