Mood disorder facts and statistics paint a picture of just how common mood disorders are in the U.S. and their economic impact.
Mood disordersare characterized by significant changes in mood that have a negative effect on daily life. While the three main states of mood disorders are depressive (depressed mood), manic (elevated mood) and bipolar (a mix of depressed and elevated moods), there are many types and subtypes of mood disorders that vary in intensity. Mood disorder statistics help paint a picture of the scope and severity of mood disorders.
Current mood disorder statistics are changing as new studies are continually being carried out. The numbers and statistics provided in this article aim to reflect the most current studies available. As time goes on, these numbers may change as new research warrants.
Prevalence of Mood Disorders
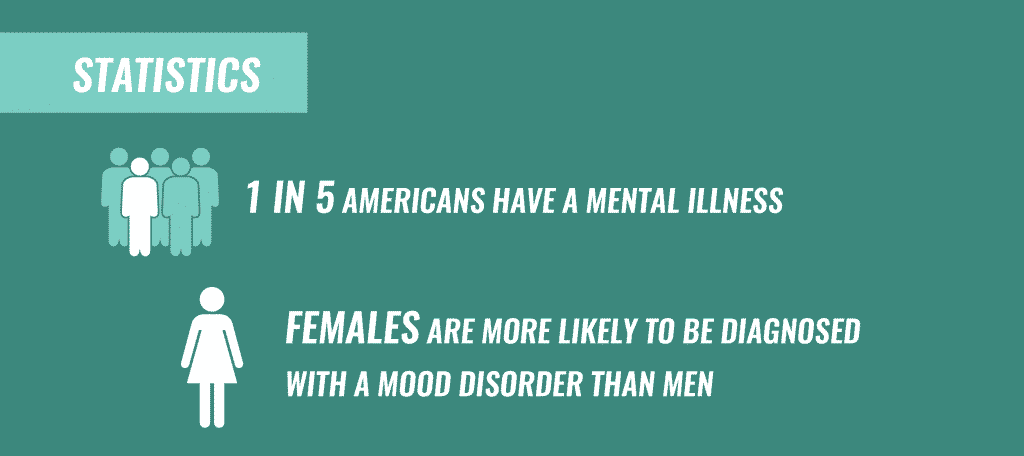
Estimates show thatnearly 1 in 5 Americanshave a mental illness, mood disorders included. Around20.9 millionAmericans adults aged 18 and older have a mood disorder.
Data from theNational Comorbidity Survey Replicationreveals the prevalence of mood disorders, showing that:
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
- Among U.S. adults 18 and older, around 9.7% had a mood disorder in the past year
- The prevalence of mood disorders in a given year was higher for females (11.6%) than males (7.7%)
- An estimated 21.4% of adults will experience a mood disorder at some point in their life
- 45% of those with a mood disorder will face severe impairment
Mood Disorder Demographics
Mood disorders can affect anyone at any point in life. Many factors can contribute to the development of mood disorders, and while some of the population may appear more vulnerable, no ethnic or age group is left out. Here are some statistics on mood disorder demographics:
Mood Disorders in Women
- A2017 studyshowed that women had a higher prevalence (22.3%) of mental illness compared to men (15.1%)
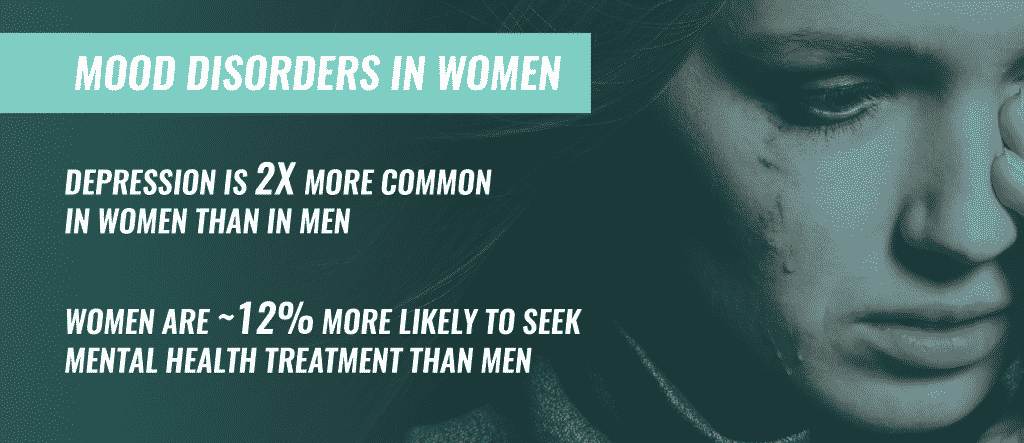
- Depression istwice as commonin women than men, with nearlyone-quarterof women experiencing a depressive episode at least once in their life
- More women (47.6%) with mental illness received treatment compared to men (34.8%), according to a2017 study
- Women with bipolar disorder have higher rates of depressive episodes and are more likely than men to receive a misdiagnosis of unipolar depression instead of bipolar disorder
Mood Disorders in Men
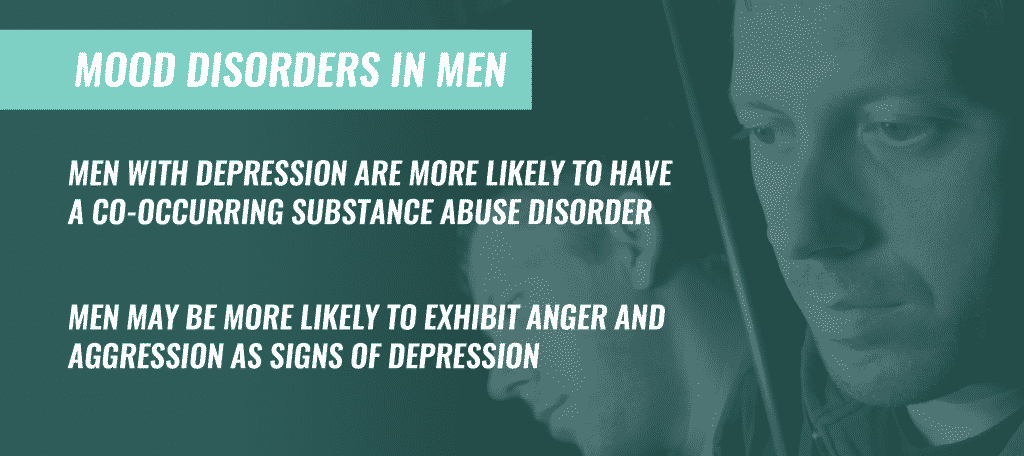
- Men are more likely to have acomorbid substance abuse disorderwith depression than women
- Men appear to be less willing than women to discuss mental health problems or seek help
- Men may be more likely to exhibitanger and aggressionin mood disorders such as depression
Mood Disorders and Age
- Half oflifetime cases of mental illnessstart by the age of 14, and 75% develop by the age of 24
- Youngadults aged 18–25have a higher prevalence of mental illness but a lower incidence of seeking treatment compared to older adults
- By the age of 18, 14.3% of adolescents will have experienced a mood disorder
Rates of Specific Mood Disorders
Mood disorders are broken down into different types based on a thorough evaluation of symptoms. Some common types of mood disorders and occurrences include:
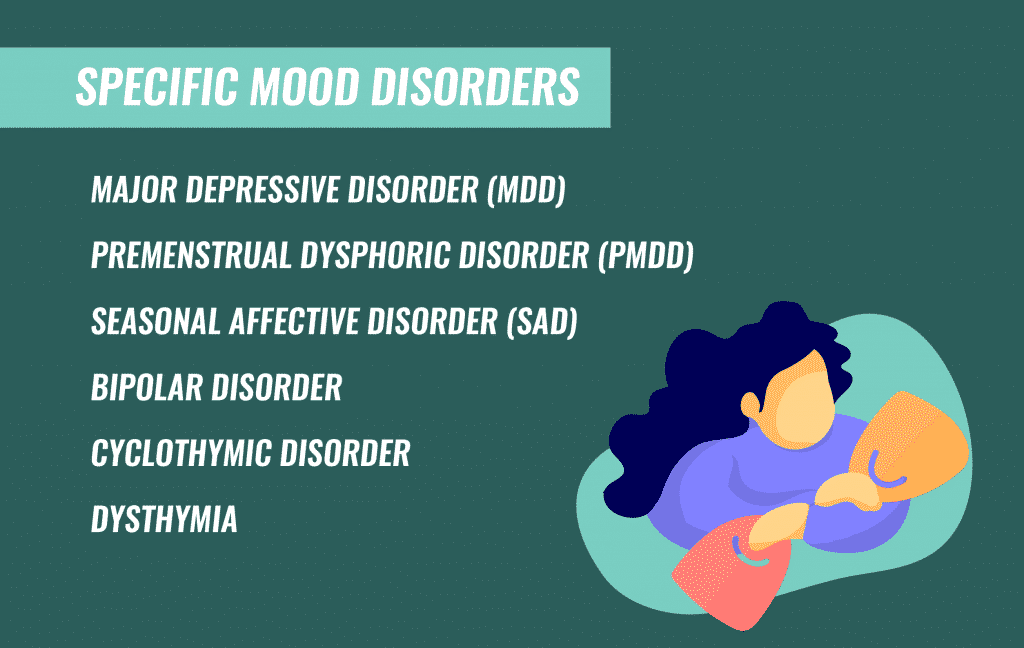
- Major Depressive Disorder(MDD):The most common among mood disorders in the U.S. is major depressive disorder. Approximately16 million Americansreported having at least one major depressive episode within the past year
- Bipolar Disorder:Currently,4.4%of US adults will experience bipolar disorder at some point in their life
- Seasonal Affective Disorder (SAD):SAD affects 10 million Americans. More than half of people with SAD have a family member with a depressive disorder, and the condition is four times more common in women than men.
- Premenstrual Dysphoric Disorder(PMDD):Around 90% of women experience PMS symptoms, 20–50% experience moderate to severe symptoms, and3–8%meet the criteria for PMDD
- Dysthymia:This form of chronic depression affects an estimated1.3–1.5%of the U.S. adult population. Of those who suffer from dysthymia,49.7%report serious impairment.
Mood Disorders and Related Health Conditions
Mood disorders can occur alone or alongside other health conditions. Certain physical illnesses may be worsened or precipitated by a mood disorder.
Some of the most common related health conditions that may be seen alongside mood disorders include:
- Personality Disorders:Mood andpersonality disorderscan appear similar, as symptoms may overlap. For instance, a person with aborderline personality disordercan experience symptoms of depression, bipolar,anxietyand substance abuse problems.
- High Blood Pressure:Research shows that people with high blood pressure are more susceptible to other cardiovascular diseases and can experience a lower quality of life, making them more at risk for psychological distress, including depression. One study linked depression and high blood pressure, concluding that 21.3% of people with high blood pressure had depressive symptoms.
- PhysicalIllness:Depression and physical illness are commonly seen together, as prolonged physical illness can trigger or increase the risk for depression. Common physical illnesses that can trigger depression and symptoms of depression include stroke, heart disease, chronic pain syndromes, and chronic fatigue.
- Multiple Sclerosis (MS):Emotional disturbances or fluctuations are common in the early diagnosis of MS. Whiledepressionis the most common mood disorder manifestation, MS and bipolar occurrence is also well-established.
Related Topic:How long does depression last?
Mood Disorders and Substance Abuse
Mood disorders and substance abuseare commonly seen together. Clinicians note that some people with mood disorders self-medicate with drugs oralcoholto combat unwanted mood disorder symptoms. Other people’s genes may make them more vulnerable to first-time drug use that leads to chronic abuse, which can eventually cause changes in the brain that lead to mood disorders.
Regardless of the cause, it’s clear that there is a strong correlation betweensubstance use and mood disorders. Research shows that:
- Among those seekingtreatment for alcoholdependence, around 20–67% had experienced depression and 6–8% had experienced bipolar disorder at some point in their lives
- Among those seekingtreatment for cocaine dependence, around 30–40% experienced depression and 10–30% experienced bipolar disorder at some point in their lives
- Individuals with depression are twice as likely to have a substance abuse problem
- People with bipolar disorder are seven times as likely to have a substance abuse problem in comparison to individuals with no mood disorders
Mood Disorders and Suicide
Having a mood disorder dramatically increases a person’s suicide risk. This fact, along with current statistics, makes seeking treatment a matter of urgency:
- Mood disorders account for one-half to two-thirds of all suicides
- Up to 90% of those who die from suicide have an underlying mental illness
- People with anxiety or depression have a 60% higher mortality rate and die an average of 8 years earlier than those without these conditions
- During major depressive episodes, suicide attempts increase 20–40 fold
Economic Impact of Mood Disorders
TheWorld Health Organizationlists depression, the most prevalent mood disorder, as the leading cause of disability worldwide. Mood disorders impact one’s ability to function in daily life and affect work performance, productivity and attendance. Mood disorder costs are complex and include direct costs for health care, medication, physician visits, and hospitalization, and indirect costs, like productivity losses, early retirement, income loss, mortality, and care-seeking.
Data from a 2010 report estimates that the global direct and indirect costs for mental disorders accumulated to $2.5 trillion. Another approach estimating the same economic burden of mental disorders in 2010 estimated the worldwide cost ofmental health disordersto be $8.5 trillion. Mental health disorders account for more economic costs than cancer or diabetes, and the cost is expected to double until 2030. In America alone, the cost of mental illness amounts to$193.2 billionin lost earnings per year. A2011 statistical reporton federal disabilityinsurancerevealed that 1,304,851 people with mood disorders received disability benefits.
Statistics on Mood Disorders Treatment and Prognosis
Mood disorders may make their first appearance early on in adolescence or teen years. However,treatmentis not usually received until several years later.
According to theNational Alliance on Mental Illness:
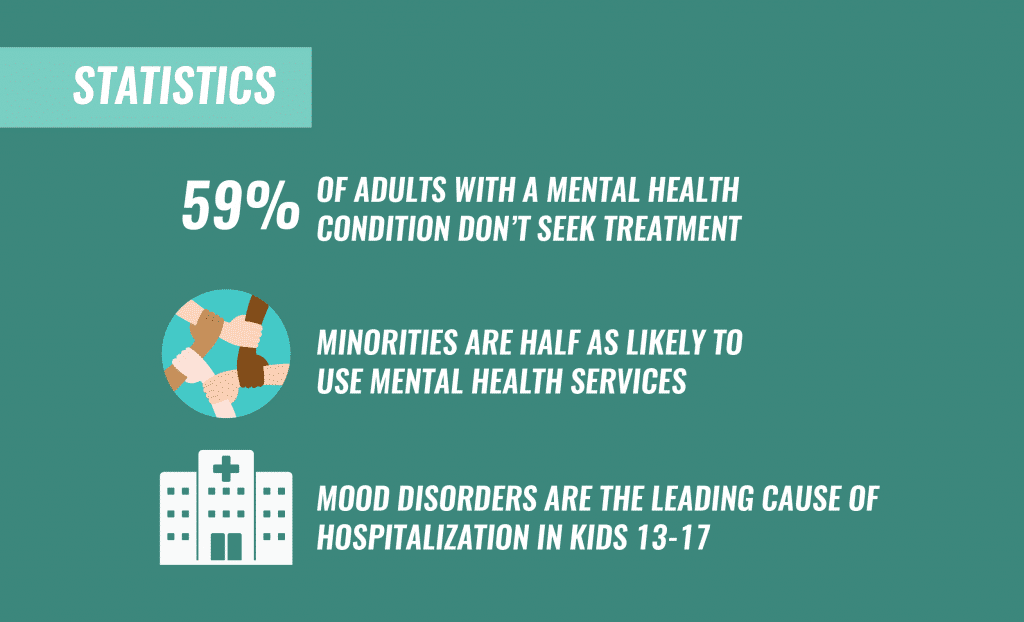
- Only 62.9% of adults who had a severe mental illness received treatment in the past year
- Only 41% of adults with a mental health condition received treatment in the past year
- Compared to Caucasians, African Americans and Hispanics used mental health services at half the rate, and Asians at one-third the rate.
Hospitalization for any condition, including mood disorders, is intensive and expensive. The rates for mood disorders hospitalizations has steadily been climbing.
Research has found that:
- Mood disorders are the leading cause of hospitalizations in children age 13 to 17
- In 2014, nearly6%of all hospitalizations were associated with mental illness or substance abuse
- In 2014, the number ofhospital staysfor mood disorders increased to 851,100, up by 23.2% compared to 2005
The prognosis for mood disorders is good, especially because doctors have a much better understanding of types and subtypes of mood disorders, includingco-occurring disordersthat could hinder treatment response. With the help of effective medication, psychotherapy or combined treatment, many people with mood disorders can lead productive lives.
If you feel that you or someone you know may be suffering from a mood disorder associated with substance abuse, please get in touch with one of our representatives at The Recovery Village.Call our 24-hour helpline todayto discuss treatment options.








