A recent survey of opioid users takes a deep dive into opioid use trends, the role of the drugs’ source, the lifelong effects of opioid use and what awaits in recovery.
While widely available vaccinations mark a positive shift in the COVID-19 pandemic, the opioid epidemic continues to affect the lives of millions of Americans. Nearly 50,000 people died from an overdose involving opioids in 2019, with the overdose death rate increasing by 38% prior to May 2020. The COVID-19 pandemic has not helped matters, as people using prescription opioids reported significant increases in their opioid use last year.
Lawsuits holding drug distributors, hospitals and thousands of other plaintiffs accountable for the impact opioids have had on public health continue to play out, with alandmark case against three of the largest drug distributorsrecently coming to trial after coronavirus-related delays.
The Recovery Village regularly conducts behavioral health research to shed light on the enduring effects of substance abuse on a person’s health, relationships and quality of life. We recently surveyed more than two thousand current or former opioid users, including those who use prescription opioids like oxycodone and illicit opioids like heroin. Exploring recent trends in opioid use, detox and recovery experiences can help raise awareness of opioid use disorder as a medical disease and better support the victims of the opioid crisis.
The Recovery Village Opioid Survey Results
The Recovery Village opioid study surveyed 2,134 American adults who formerly or currently use prescription opioids, illicit opioids or a combination of the two. We asked them about their opioid use, related outcomes, health and more. In addition, 1,866 respondents had undergone opioid withdrawal, so we asked them about their recovery. Of these, 1,200 participants answered questions about their time in a rehabilitation treatment facility. Note: Some questions asked respondents to select each option that applied, so the total percentage will be greater than one hundred in a few cases.
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
Opioid Use Stats
Prescription opioid users make up the majority of people impacted by these substances, with only 39% using the illicit drugs heroin and opium. Roughly 25% of users reported using fentanyl, which includes illegally manufactured fentanyl and approved drugs like Duragesic and Fentora. The most popular opioid among our respondents was oxycodone, prescribed by doctors under the brand names OxyContin, Percocet or Percodan, with 68% reporting using it.
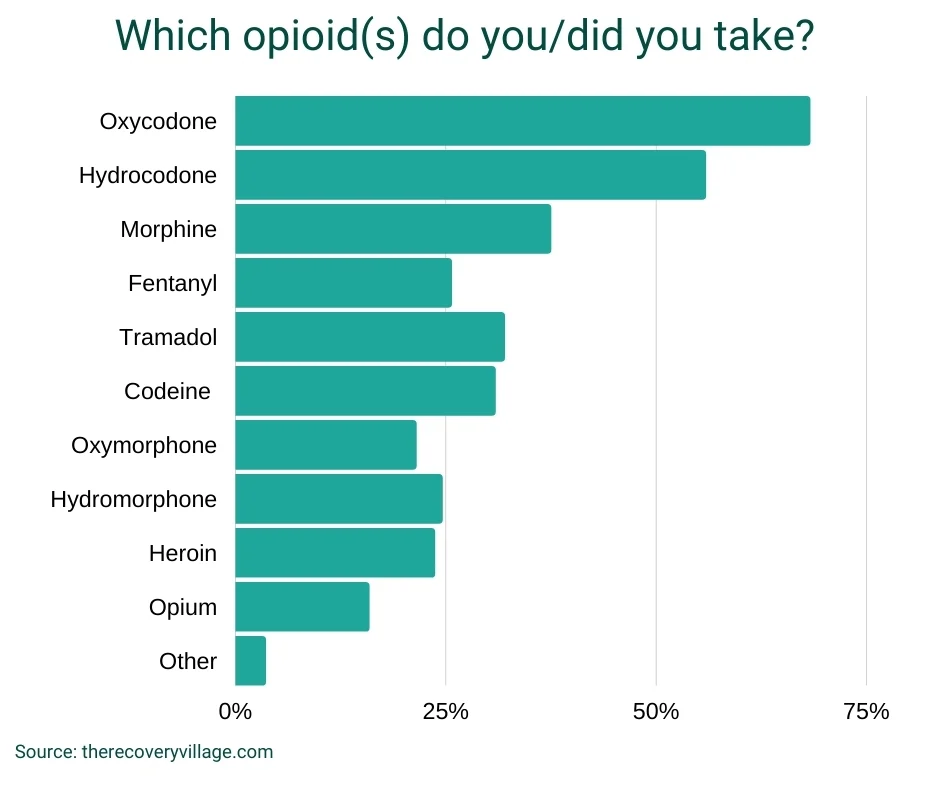
Notably,72% of respondents had taken multiple kinds of opioids, with 24% having used five or more different opioids. Five percent of respondents had used widely, reporting use from every opioid listed.
Respondents hada variety of reasons for using opioids, prescription or illicit:
- 57% used opioids to deal with chronic pain
- 42% used opioids to cope with an injury
- 52% used opioids to feel a “high” or euphoria
- 40% self-medicated their mental health symptoms with opioids
- 41% used opioids to deal with stress
- 28% used opioids recreationally
- 17% used opioids because of a family member or loved one’s influence
Another 24% reported experiencing cravings for opioids and 13% reported physical dependence. In these circumstances, it can be difficult and uncomfortable to stop opioid use on your own. It also doesn’t take long to get here. Among those studied, 87% had undergone an opioid detox, yet 51% of respondents had been using opioids for six months or less. Only about 14% of respondents had been using opioids for more than five years.
The Path to Opioid Abuse
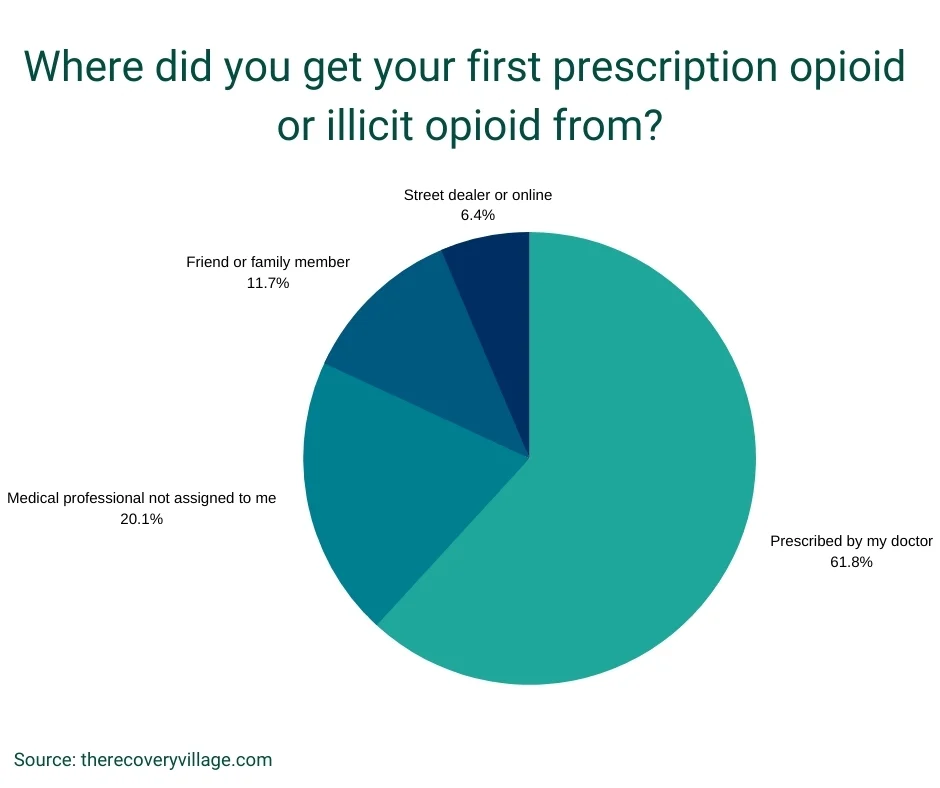
More than half (57%) of those surveyed were introduced to opioids through their doctor or other healthcare professional as part of an official prescription they used as directed.
However, the wide availability of prescription opioids has made opioid misuse relatively easy. Misuse, including behaviors like using someone else’s prescription, getting a falsified prescription, and “doctor shopping” for a prescription that is no longer medically necessary accounted for 34% of respondents’ first opioid use. Only 9% of participants said they started their opioid use with an illicit opioid like heroin or opium.
The opioid crisis is often painted as individuals making bad decisions and over-using their prescriptions, but that just isn’t the case for many. When asked to describe their opioid use history,41% received opioids through a legitimate means (their doctor’s prescription)and always used them as instructed. Even these individuals reported negative impacts on their quality of life and ran a severe risk for addiction.
- 1 in 3 respondents started with a legitimate need for a prescription opioid and eventually transitioned into misusing other prescription opioids or going to illicit opioids like heroin.
Where did opioid users obtain their opioids? The majority of users got their drugs from a regulated source (62%), with street dealers only accounting for 6% of users.
One in five users get their opioids illegally from a medical professional(a doctor or pharmacist, for example) who is not assigned to them. These bad actors in the medical community perpetuate the opioid crisis, often for their own use or monetary gain.
Opioids and Polysubstance Abuse
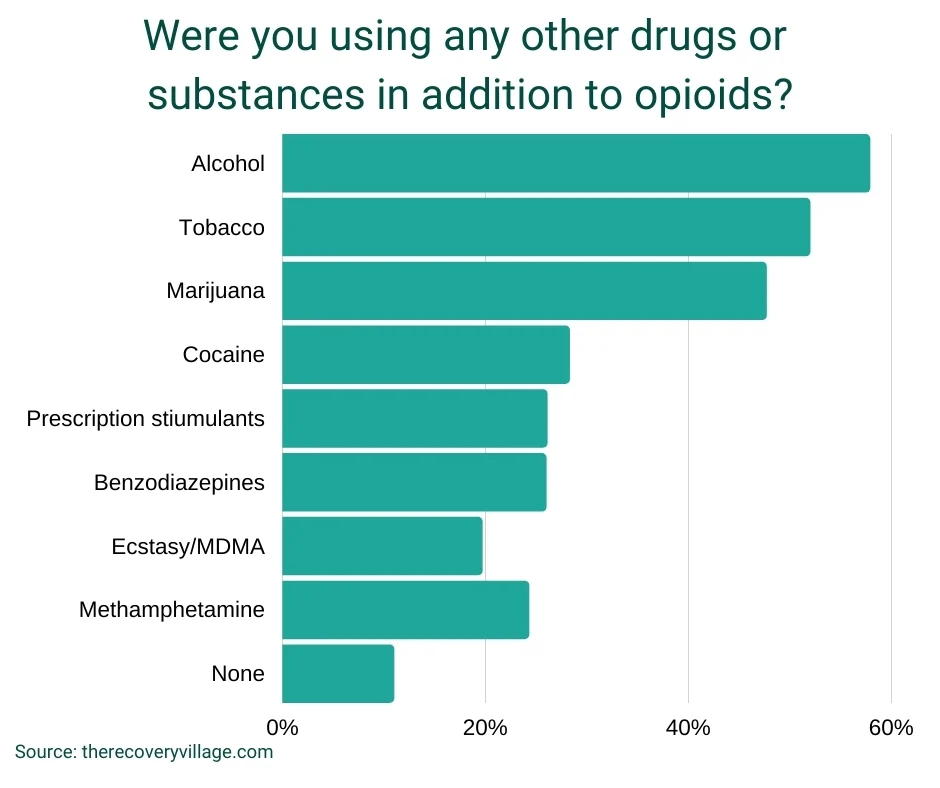
Using multiple substances, called polysubstance abuse, can put people at greater risk of a deadly overdose, adverse side effects, health complications and a more complicated, dangerous detox process. Among recorded overdose deaths from a synthetic opioid in 2016,80% involved another drug or alcohol. The vast majority(89%) of opioid users are using some other substance in addition to opioids, putting themselves at greater risk.
Opioids and Their Impact
Opioid use, misuse, dependence and addiction can impact every facet of your life. While opioids may offer pain relief, relaxation or an enjoyable high, many of our respondentsreported negative impacts that may have outweighed these benefits. Among those surveyed:
- 50% reported impacts to their mental health
- 46% reported impacts to their physical health
- 46% reported opioids affected their relationships with their loved ones
- 45% reported their finances were impacted
- 37% reported impacts to their career/job
- 37% reported impacts to their appearance/hygiene
- 35% said opioids impacted their parental abilities
- 16% had a legal issue (arrest, incarceration or a fine)
Medical Emergencies
Using heroin or misusing prescription opioids can lead to a medical emergency. Opioid overdose is a common and often fatal part of the opioid crisis, accounting for 70% of all drug overdose deaths. Overdose complications are usually tied to respiratory depression, where the person can’t circulate enough oxygenated blood, leading to unconsciousness, brain damage, coma and death. Among those surveyed:
- Nearly half (48%) had been to the hospital for a medical emergency directly related to their opioid use (usually an overdose).
- 1 in 3 respondents (37%) had overdosed without getting to medical care in time.
- 1 in 3 respondents (34%) had received the opioid antidote naloxone (Narcan) for an overdose, which binds to the opioid receptors to get oxygen back into the blood.
People who were taking a prescription opioid that was prescribed to them were 67% more likely to have an emergency hospital visit than people taking an opioid they received illicitly. While this sounds high, it may mean that people already working with their doctor were more likely to get medical help when an emergency or overdose occurs.
In contrast, people who received their opioid illegitimately, like from a doctor or pharmacist giving them a fake prescription or under-the-table drugs, weretwo times more likely to overdose without getting medical care.
Obviously, this study includes people who experienced either a close call or non-lethal impacts. We would expect many of these figures to be much higher if also accounting for opioid users who did not survive the effects of their use.
Long-term Health Complications
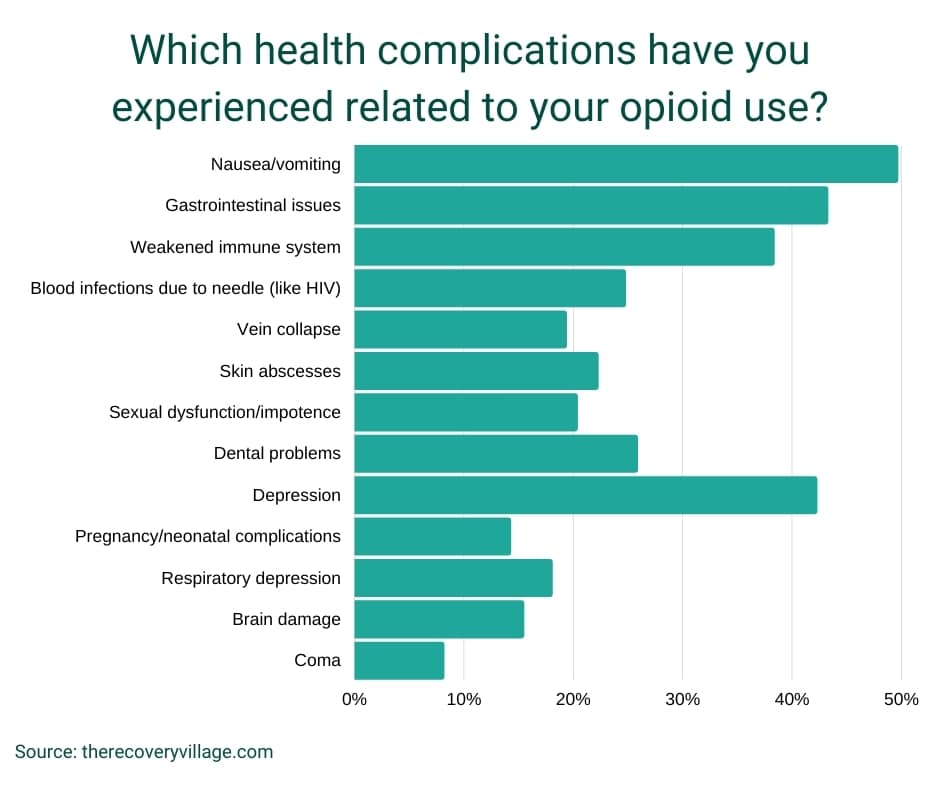
Opioid use can have lasting impacts on your health, even if you manage to avoid an overdose. Among those surveyed, the most common health complications directly related to opioid use were having nausea or vomiting (50%), gastrointestinal issues (43%) and depression (42%).One in ten opioid users reported going into a coma from their use.
Opioids received from street dealers are often unpredictable and more dangerous. People who used these opioids were 53% more likely to enter a coma than other users and 25% more likely to have brain damage.
Finding Help for an Opioid Addiction
Most opioid users eventually see their opioid use as a problem they want to address:4 out of 5 opioid users (80%) wanted to get outside help for their substance use. The largest group (39%)preferred professional treatment through a rehab facility like The Recovery Village. Another 18% chose a support group for guidance on their recovery journey, and 17% said they would or did work with their doctor. A small number wanted government-backed voucher programs that offered cash incentives for sobriety (6%).
Barriers to Treatment
In this study, 17% of participants stated they would not seek any help and try to recover from opioids on their own, while 3% would not stop at all. When asked to rank reasons why they wouldn’t get help for opioid use, the top reason was a fear of returning pain. While pain can be a powerful demotivator, many people in recovery get help managing their pain without opioids.
The financial cost, uncertainty about treatment and family obligations were other barriers to treatment for opioid users. This website can help you navigate insurance for rehab, learn more about opioid addiction treatment and how to help your family cope.
Opioid Detox and Withdrawal Stats
When someone stops using opioids, the body begins to remove all of the drug left in its system in a process called detoxification. Detoxification often comes with uncomfortable or sometimes dangerous opioid withdrawal symptoms that can lead to relapse. Detoxing under medical supervision helps manage your withdrawal symptoms so that you’re as safe and comfortable as possible.
The vast majority (89%) of participants reported detoxing from an opioid at some point in their lives: 7 out of 10 decided to detox at home (71%), while 29% decided to undergo a medical detox at a rehab center or medical facility.
The amount of time it can take to completely detox from opioids varies depending on the person’s physiology, opioid use and other factors. In general,95% of the opioid users surveyed experienced withdrawal symptoms for 2–8 days. The most common withdrawal length was three days.
People who underwent detox for opioids (either at home or at a facility)reported experiencing many different withdrawal symptoms.
- 4 in 10 participants reported nausea and vomiting (43%)
- 4 in 10 participants reported muscle cramps (42%)
- 4 in 10 participants reported insomnia (42%)
- 4 in 10 participants reported hot flashes (40%)
- 3 in 10 participants reported sweating, teary eyes or a runny nose (38%)
- 3 in 10 participants reported diarrhea (38%)
- 3 in 10 participants reported high blood pressure (35%)
- 3 in 10 participants reported rapid heartbeat (33%)
- 1 in 4 participants reported paranoia (29%)
- 1 in 4 participants reported dilated pupils (24%)
- 1 in 4 participants reported hyperactivity (28%)
Heightened anxiety was the most commonly reported opioid withdrawal symptom (56%).
Opioid Rehab Treatment Stats
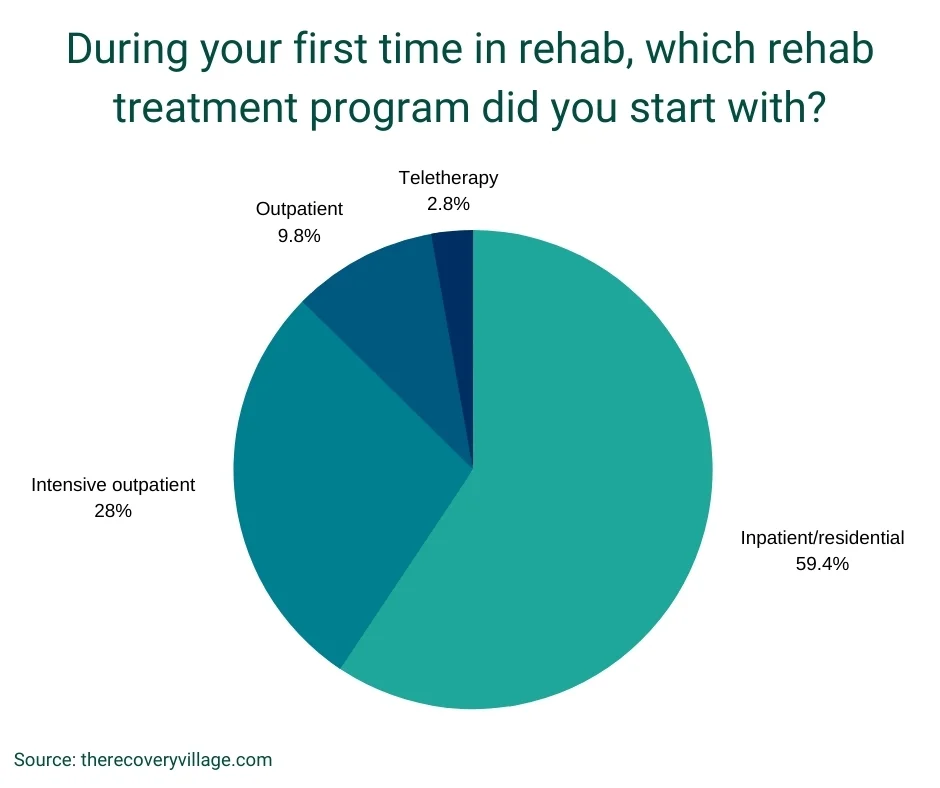
Opioid addiction treatment at a rehabilitation facility is an evidence-based path to recovery. Among those surveyed, 56% reported attending rehab treatment. Most rehab patients in this study spent their first time in the highest level of rehab treatment: inpatient or residential care (59%). Beginning treatment at more intensive levels of care and progressing to less intensive programs, utilizing the full continuum of care, leads to better recovery outcomes.
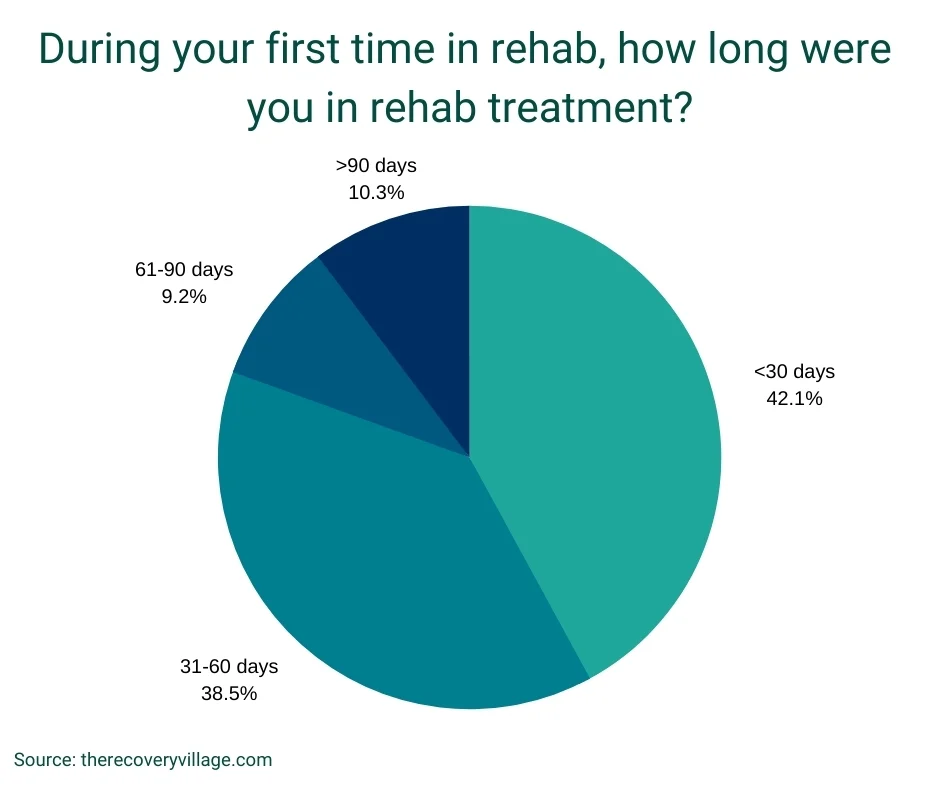
Spending more time in rehab is also associated with better outcomes. Outpatient programs generally last longer than inpatient care, but programs may vary significantly or be tailored to the individual’s needs. Among the opioid users surveyed,4 out of 5 spent less than two months in rehab (81%).
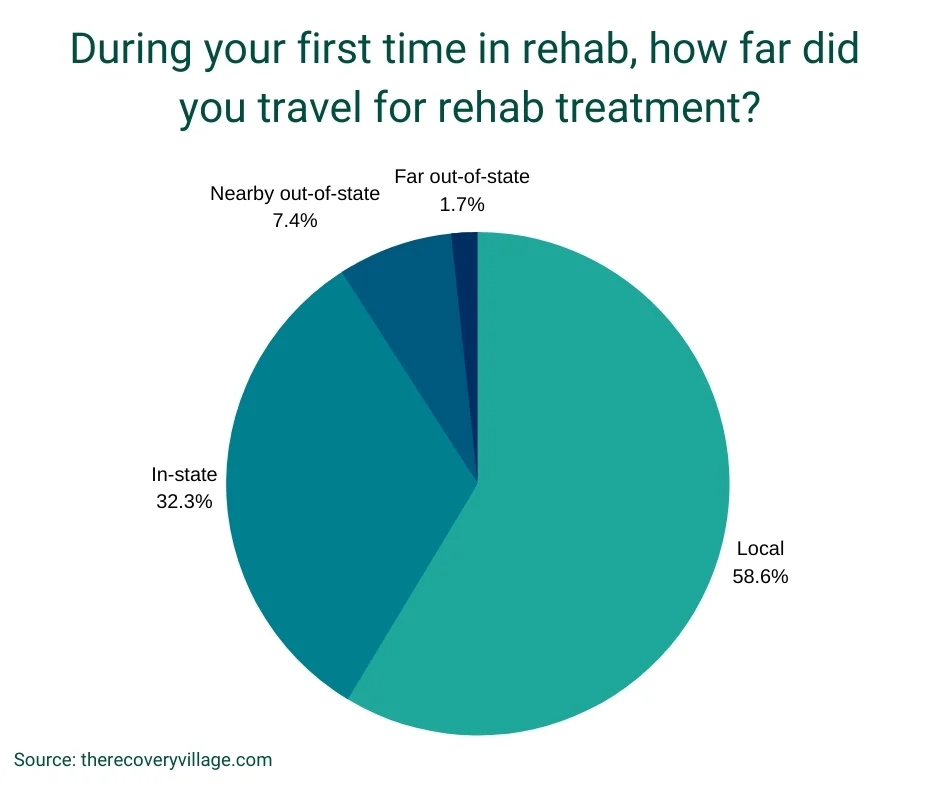
Due to the widespread nature of the opioid crisis, opioid addiction treatment programs are readily available across the country. However, some people entering recovery from opioids may travel to another city or state to find a program that meets their unique needs.
Among the rehab patients surveyed,87% reported finishing their first treatment program completely. Finishing your treatment program significantly raises your chances for good recovery outcomes and lowers your chance of relapse while leaving early does the opposite. Specifically,people who received their opioids through a legitimate prescription by their doctor were 95% more likely to finish their rehab program, most likely due to the medical support they received prior to their rehab treatment.
However, recovery is a lifelong experience, so it is not uncommon to attend rehab treatment more than once over the course of one’s lifetime. Among the surveyed patients who attended a rehab:
- Four out of every five people attended rehab multiple times.
- Half of the participants (56%) attended rehab three or more times.
Relapse & Long-Term Recovery
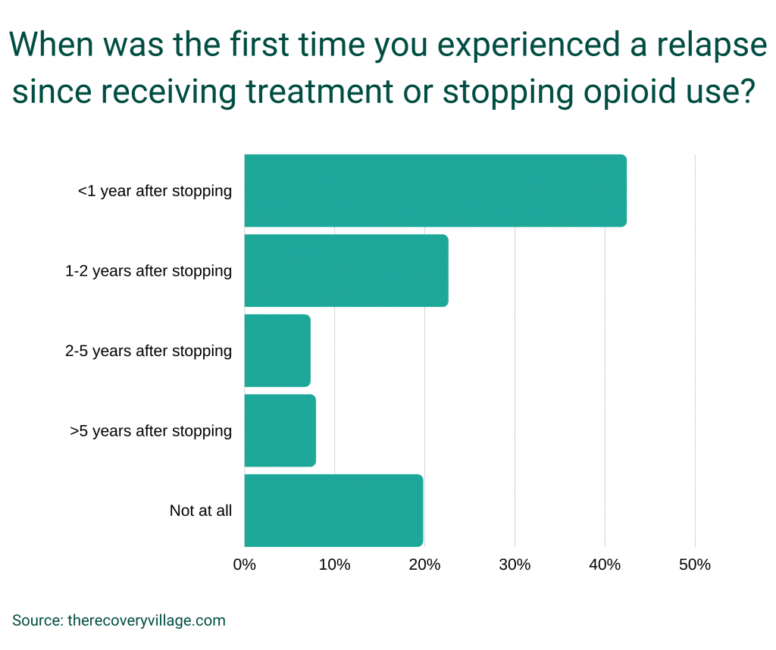
Relapse is a common and normal occurrence during recovery, and it doesn’t mean failure.Four out of five participants reported relapsing after they started their recovery (80%), with 42% doing so within the first year.
Many people relapse more than once throughout their lifetime in recovery from opioid use, leading to multiple returns to rehab. Opioid addiction is not easy to recover from, but it is possible.
- Most commonly, 24% only relapsed once so far.
- More than half (56%) had relapsed three times or less.
- Roughly 14% reported relapsing more than ten times over their lifetime.
Though relapse is common, it is not unavoidable. Attending rehab treatment gives you access to relapse prevention planning and aftercare resources that can help you stay opioid-free for longer and longer periods and improve your quality of life. For those struggling with opioid addiction, these are true measures of long-term recovery.
Recovery From Opioid Addiction Is Possible
If you or a loved one struggles with a dependence on opioids, know you’re not alone. This study shows thousands of people across the country started with a legitimate prescription for an opioid but became dependent or addicted, experiencing dangerous overdoses and negative impacts on their health and quality of life. Most survey participants choose to end their opioid use through rehab treatment, and a majority have been to rehab multiple times throughout their recovery.
While the recovery journey for opioid addiction is not easy, living a life free from opioids is possible. Our helpful representatives can answer questions about what rehab is like, how insurance can help cover costs, and how to care for your family in the meantime. Whether it’s your first time in treatment or not, contact us today to learn about our evidence-based addiction treatment programs and long-term recovery resources.
Methodology
Surveys conducted by The Recovery Village use an organic, random sample of U.S. Americans collected throughPollfish’s random device engagement (RDE)sampling method. All surveys are double-blind studies with a 95% confidence interval and ±3% margin of error.
In this survey, the sample size for general opioid questions was 2,134. The sample size for detox- and recovery-related questions was 1,866, and the sample size for rehab-related questions was 1,200. The requisite sample size was determined based on the estimated national population size of adult prescription opioid and heroin users (18+) in the2019 National Survey on Drug Use and Health.
Survey questions were developed usingspecificationsanddefinitionsfrom the Substance Abuse and Mental Health Services Administration (SAMHSA) and National Institute on Drug Abuse (NIDA), as well as insights from addiction experts and medical professionals.








