Tourette Syndrome is a complex condition involving involuntary tics. Learn more about Tourette’s symptoms, causes and risk factors.
Tourette syndrome, or Tourette’s, can be a difficult condition to live with, but it is manageable with the right care. The symptoms of Tourette syndrome, namely verbal tics, may inhibit a person’s daily life, but with a proper medical diagnosis, solid treatment plan and a strong support network, a person with Tourette’s can lead a fulfilling life.
What Is Tourette’s?
According to the National Institutes of Health, Tourette syndrome is a neurological condition that involves automatic, unconscious movements and utterances called tics. Tourette disorder usually begins in early childhood in the range of 3 to 9 years of age, with cases of Tourette’s occurring more often in males compared to females. It is common for individuals with Tourette’s to experience areduction in symptoms as they age, with Tourette’s improving during the late teenage years and early twenties.
Symptoms of Tourette’s
Tourette’s symptoms include both simple and complex tics, which can be either motor tics or verbal tics.
Simple Tics
Simple motor ticsthat occur in Tourette syndrome include movements that involve only a few muscles, such as blinking the eyes or shrugging the shoulders. Simple tics can also involve vocalizations, such as grunting or clearing the throat repeatedly.
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
Additional examples of simple tics that may occur in Tourette syndrome include:
- Grimacing
- Twitching
- Opening the mouth
- Eye rolling
- Snorting
- Sniffling
Complex Tics
The complex tics that occur with Tourette’s are more distinguishable than simple tics are, and they involve the movements of multiple muscle groups or the production of vocalizations that include longer phrases. Sometimes complex motor tics in Tourette’s involve a combination of movements, such as shrugging the shoulders and then blinking and turning the head to the side.
Some individuals who experience Tourette’s may engage in complex motor tics that involve some form ofself-harm, such as hitting oneself. Complex tics can also involve actions such as touching items, hopping or tapping the feet. In addition, complex verbal tics could involve repeating phrases, including what other people say or inappropriatephrases that contain profanity.
Causes of Tourette’s
While the exact cause of Tourette syndrome remains unclear, scientists have researched risk factors that could potentially contribute to the development of Tourette’s. According to theCenters for Disease Control and Prevention (CDC), Tourette syndrome has a genetic basis and is likely the result of multiple genes working together.
Risk Factors
TheCDCreports the following Tourette’s risk factors:
- Being male
- Abnormal metabolism of the neurotransmitter dopamine
- Maternal cigarette use during pregnancy
- Certain infections
- Pregnancy-related complications
- Low weight at birth
Diagnosing Tourette Syndrome
A medical professional can diagnose Tourette syndrome with theDiagnostic and Statistical Manual of Mental Disorders,fifth edition (DSM-5). To meet diagnostic criteria from the DSM-5, a person must engage in at least two motor tics and one or more vocal tics.
For example, a person diagnosed with DSM-5 Tourette’s may demonstrate facial grimacing, blinking and grunting, but the different tics do not need to occur simultaneously to meet diagnostic criteria. Additional criteria necessary for diagnosing Tourette’s via the DSM-5 include the onset of the tics being prior to the age of 18, and the tics need to occur for at least a year. Tics that occur as a result of taking medication or being diagnosed with another medical condition do not meet DSM-5 diagnostic criteria for Tourette’s.
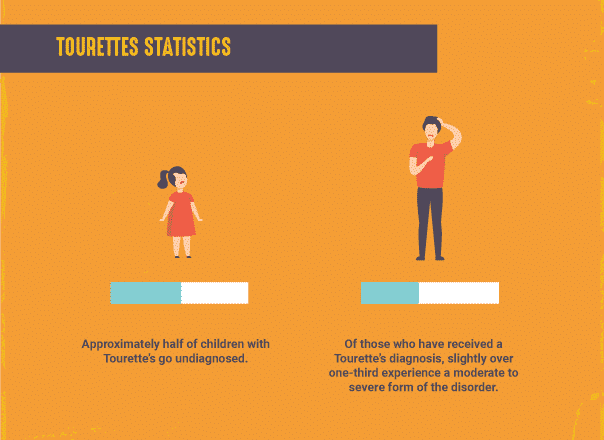
Tourette’s Facts & Statistics
TheCDCcompiles and presents data on Tourette syndrome.According to the data, Tourette’s occurs in less than one percent of American children, with an estimated 1 out of 162 children experiencing the condition. Furthermore, approximately half of children with Tourette’s go undiagnosed. Of those who have received a Tourette’s diagnosis, slightly over one-third experience a moderate to severe form of the disorder.
Tourette syndrome statistics indicate that this diagnosis is more common in the following groups:
- Males
- Non-Hispanic Whites
- Those aged 12-17 (when compared to ages 6-11)
Tourette’s and Co-Occurring Disorders
It is not unusual for individuals with Tourette’s to experience othermental healthconditions, includingattention-deficit hyperactivity disorder (ADHD). According to the research, Tourette’s and ADHD often occur together, with data from theCDCshowing that 63 percent of children with Tourette’s are also diagnosed with ADHD.
Tourette’s andanxietyare also likely to co-occur, with 49 percent of children with Tourette’s also demonstrating difficulties with anxiety.Obsessive-compulsive disorderis present in over one-third of children with Tourette’s. Furthermore, Tourette’s and depression occur together in one-fourth of children with Tourette’s.
Other mental and cognitive diagnoses associated withTourette syndromeinclude:
- Behavioral issues
- Conduct disorders
- Autism
- Learning disabilities
- Developmental delays
- Intellectual disabilities
- Difficulties with speech and language
Beyond these conditions, children diagnosed with Tourette’s are more likely to experience other health problems, such as asthma or conditions involving the muscles or joints. Researchers writing for theJournal of Child Neurologyalso caution that Tourette’s can be associated with anelevated risk ofsubstance abuse, perhaps because of co-occurring conditions ordual diagnoseslike ADHD. In addition, teens with Tourette’s may experiment with drugs andalcoholto control their tics.
Tourette’s Treatment
Tourette syndrome treatmentcan involve psychological interventions, medication or both. As the National Institutes of Health has reported, there are effective medications available to treat tics that interfere with daily life. Neuroleptic drugs, such as haloperidol and pimozide, have demonstrated effectiveness in Tourette’s treatment. While these medications do have side effects, they can be managed with the help of a physician. Not all individuals who have Tourette’s will require medication totreat their condition.
Children with co-occurring ADHD and Tourette’s may benefit from taking medications. A 2002 study in the journalNeurologyfound that the combination of the medicationsclonidineandmethylphenidatewas effective for treating ADHD among patients with Tourette syndrome, and the medication did not increase the occurrence of tics when compared to a placebo.
Behavioral interventions can be effective for treating Tourette’s, either on their own or as an adjunct to medication. In areview of multiple studiesthat assessed the effects of behavioral therapy as a form of Tourette syndrome treatment, researchers affiliated with the University of South Florida and the University of California Los Angeles found that this type of therapy has moderate to large beneficial effects.
The researchers determined that behavioral therapy is an effective Tourette’s treatment, especially when patients attend more therapy sessions. Behavioral therapy was also found to be more effective among patients without co-occurring ADHD. As theNational Institutes of Healthhas explained, psychological interventions may be a helpful Tourette’s treatment because they provide a person with the support he or she needs to manage the disorder and to cope with any co-occurring mental or emotional health issues.
If you or someone in your life struggles with drug or alcohol use and co-occurring Tourette’s, The Recovery Village can provide services that address these challenges. The Recovery Village has facilities invarious locations across the country, offering comprehensive addiction treatment in addition to services to treat co-occurring conditions. For more information,contact a representativetoday.









