Rumination is a negative thought cycle that many people struggle to manage. This is an overview of the causes and co-morbidities of rumination.
Rumination is a thought processing disorder meaning that worrisome thoughts or even neutral thoughts are given excess analysis by the person who ruminates. Sometimes, a person is able to stop the recycling of the thoughts and move on to other activities or other thoughts, whereas in more severe cases, the person cannot break out of the thought process. This cycling of thoughts can lead to other dysfunctional behaviors or disorders.
Rumination, the thought disorder, is not to be confused with “rumination disorder,” an eating disorder involving regurgitation of food. For more information on rumination disorder, see ourrumination disorder overview page here.
What Does it Mean to Ruminate?
Rumination is defined as excessive, repetitive thinking about the same event. Rumination is divided into two subtypes, reflective and brooding. Reflective is a cycle of thinking that is analytical and problem-solving, whereas brooding is more negative and self-perpetuating. Brooding rumination leads to negative moods and negative opinions of oneself. Brooding can also lead to substance abuse or other mental health problems, includingdepressionandanxiety.
The reflective form of rumination is generally viewed positively in that it provides a chance for the person to reflect on behaviors and consequences and not let past events ruin their day. However, both forms of rumination can be associated with depression, anxiety and substance abuse.
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
Signs and Symptoms of Rumination
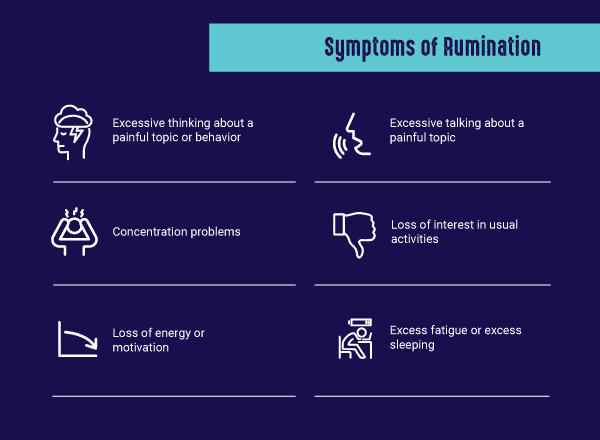
Rumination is a major component of depression. Rumination, especially brooding, may make a person prone to depression and make therapy less effective.Signs of depressionare also signs for rumination and include:
- Excessive talking about a painful topic
- Excessive thinking about a painful topic or behavior
- Sadness
- Numbness
- Irritability
- Mood swings
- Concentration problems
- Loss of interest in usual activities
- Loss of energy or motivation
- Feelings of worthlessness or helplessness
- Excess fatigue or excess sleeping
- Appetite disturbances
- Suicidal thoughts
What Causes Ruminating Thoughts?
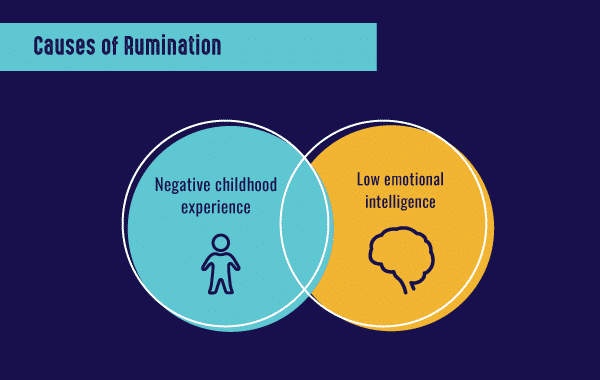
Coping styles such as toxic brooding or rumination may be due to negative experiences in childhood or adolescence that cause a person to have trouble coping with their thoughts. Rumination is a style of coping that is mostly counterproductive until it is replaced with more positive coping styles. Since the peak onset of mood disorders,substance abuseand psychosis are during adolescence and teenage years, rumination styles parallel the onset of functional or dysfunctional behaviors that reinforce if not dealt with before becoming self-fulfilling.
Emotional intelligenceis affected by brooding and reflective rumination. Brooding rumination is associated with a lower emotional intelligence whereas reflective is more commonly found with higher emotional intelligence scores. Furthermore, suicidal thoughts are more common in individuals that have low emotional intelligence and rumination.
Positive or negative coping may determine the type of rumination.Active copingis associated with more of a reflective form of rumination, a higher emotional intelligence, and less depression. The opposite is seen in brooding rumination where there are lower emotional intelligence and higher rates of depression.
Rumination Statistics
Specific statistics are difficult to determine due to the nature of rumination. Because rumination is commonly seen in people who experience depression and anxiety, some people with these two disorders may also experience rumination at some point in their lives.A study from the University of California, Riverside showedthat people who experience rumination may delay seeking treatment for serious medical conditions such as breast or colon cancer, which could cause people experiencing rumination to have higher health risks than those without rumination who seek treatment right away.
Rumination and Co-Occurring Disorders
There is evidence thatdepressive ruminationis seen as symptoms in other disorders besides depression. The most common co-occurring disorders seen with rumination are social and generalized anxiety disorders and substance abuse.
Additional conditions associated with rumination include the following:
- Bulimia
- Binge eating disorder
- Obsessive-compulsive disorder
- Post-traumatic stress disorder
- Personality disorders such as borderline personality disorder
Eating disorders, such as bulimia and binge eating disorder, that often co-occur with rumination are a challenge to treat until the negative thoughts are addressed and replaced with positivity.
Treatment for Rumination
Rumination treatmentaims to redirect the thought process and improve coping skills and address the associated depression or anxiety.Rumination-focused cognitive behavioral therapy(RFCBT) is a psychobehavioral therapy targeting rumination.
RFCBT iscompared tocognitive behavioral therapy (CBT)in depressed patients who are not responding or benefitting from current behavioral therapy or counseling. The goal of RFCBT is to develop strategies to promote concrete and specific thinking by modifying the thought process, whereas CBT tries to modify the content of thinking.
Unlike RFCBT that is primarily used to treating moderate to severe ruminators, CBT for rumination has shown promise especially for those with mild rumination scores. CBT is more useful for single negative thoughts rather than ongoing and successive ruminations that build upon each other. CBT aims to disrupt the vicious cycle of negative thought.
Mindfulness exercises for rumination start with the identification of the event in question, acceptance that something negative has occurred, facing the truth of the matter honestly, being creative and curious about how to solve the negative thought, being thankful for all the good things in your life and having inner self-control. Walks in nature, yoga and other relaxation techniques are forms of mindfulness. Exercise, vitamins, herbs and essential oils in aromatherapy may provide added benefits.
Medications include those that treat co-occurring conditions such as depression and anxiety. Common medications include:
- Selective Serotonin Reuptake Inhibitors (SSRIs)– Some common SSRIs areProzacandPaxil. Serotonin is a chemical or neurotransmitter in the brain responsible for mood and is one of the four happy hormones, norepinephrine, GABA, and dopamine. The exact mechanism is unknown but they help maintain healthy levels of serotonin by preventing serotonin from being degraded in the brain.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)– These are used to treat anxiety, depression and panic disorder. They impact both serotonin and norepinephrine levels in the brain. They are useful for people who have excessive rumination.
- Benzodiazepines–These are anti-anxiety medications that are helpful in addressing underlying anxiety associated with rumination on a short-term basis.
If you or a loved one misuse substances to self-treat for rumination, consider seeking treatment. At The Recovery Village, patients receive individualized treatment plans that address addiction and any co-occurring substance use disorders.Call a representative todayto learn more about the treatment process and take the first step toward a healthier future.








