Rumination disorder is a difficult eating disorder to cope with characterized by regurgitating food. Learn more about the disorder and treatment option.
Rumination disorder is a type ofeating disorderthat is somewhat rare in the United States. Sometimes called rumination syndrome, this condition involves regurgitating food and is common among infants. Fortunately, treatment options exist for rumination eating disorder, and the condition can be managed successfully.
What Is Rumination Disorder?
Rumination disorder, or rumination eating disorder, is characterized by the regurgitation of food, possibly re-chewing it, and then re-swallowing the food. For the person who has this condition, rumination disorder is relatively effortless, unlike vomiting which requires forceful abdominal muscle contractions. In an infant who has this condition, they may roll their tongue and arch their back during the episode.
Also known as rumination syndrome, this condition is thought to represent a motility disorder with involuntary relaxation of the muscles that control the opening and closing of the esophagus.
Who Is Affected by Rumination Disorder?
Infants are most commonly affected by rumination disorder, and the age of onset is usually between three and 12 months. Infants tend to outgrow the syndrome, but some people carry these behaviors into adulthood. It is quite uncommon, but the exact incidence is unknown because adolescents and adults may hide the behavior out of embarrassment.
Treatment Can Be Life Changing. Reach out today.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
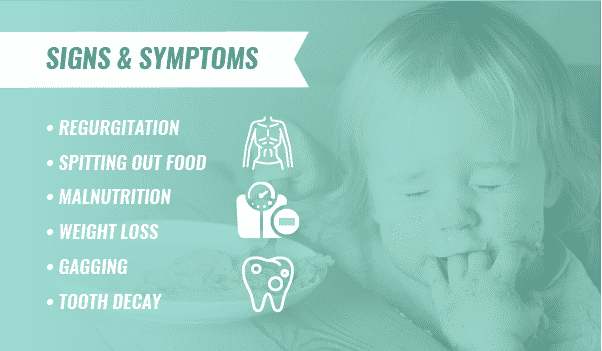
Signs and Symptoms of Rumination Disorder
Rumination disorder signs and symptomsmay include:
- Regurgitation
- Spitting out food
- Malnutrition
- Weight loss or failure to thrive
- Putting hands to mouth before regurgitation
- Gagging
- Tooth decay
- Bad breath
- Choking
- Chapped lips
Effects of Rumination Disorder
Many effects of rumination disorder result fromfood and acid returning to the mouth. These effects and other rumination disorder health risks may include:
- Bad breath
- Tooth decay
- Malnutrition
- Weight loss
- Chapped lips
- Loose esophageal sphincter
- Acid reflux
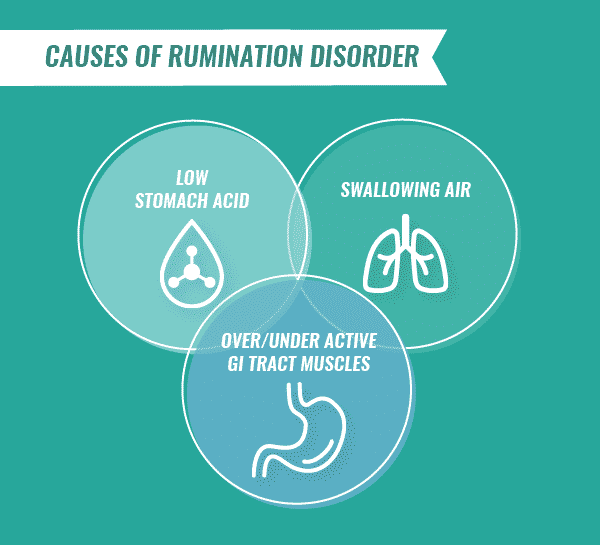
Causes of Rumination Disorder
The causes of rumination disorder cannot always be determined. There may be multiple underlying reasons, such as a weakened esophageal sphincter that readily permits food contents from the stomach to return to the mouth.
Cultural, socioeconomic and psychological factors are the most commonly cited causes of rumination disorder. Specifically, the bond between mother and infant may be impaired from maternal neglect or from an overstimulated, chaotic environment.
Other theories surrounding the cause for rumination disorder are based on negative or positive reinforcement. Increased attention from other people as a response to the regurgitation, or to cure boredom may be other causes. Psychiatric disorders such asdepressionandanxietymight be other causes of rumination disorder.
Physical conditionsmay predispose a person to rumination disorder. Some of these conditions include:
- Gastroesophageal reflux (GER)
- Belching or heartburn
- Over- or under-active muscles of the gastrointestinal tract (spasms)
- Abnormal tongue movements
- Low stomach acid
- Poor chewing
- Swallowing air
- Hand or finger sucking
Diagnosing Rumination Disorder
Rumination disorder diagnosisis based on blood tests to check for anemia or electrolyte abnormalities. Anemia may occur due to damage to the stomach or esophageal walls. Imaging studies are done to diagnose rumination disorder or other predisposing conditions. A barium swallow can show a hiatal hernia, narrowing of the esophagus and abnormal motility of the esophagus or stomach.
An upper gastrointestinal (GI) series and small bowel follow-through test can diagnose an ulcer or other mechanical or physical problems of the intestines. Other lab tests that may be helpful are cultures for Heliobacter pylori (which is a bacteria that causes ulcers), studies to measure the rate of stomach emptying, motility, pH testing and X-rays.
Rumination diagnosis is based uponruling out other gastrointestinal conditions, and the condition must be present for one month.
Risk Factors for Rumination Disorder
The main risk factor for rumination disorder is beinginstitutionalized due to profound intellectual disability. People of average intelligence can develop rumination disorder, but due to the secretive nature of the disorder in adults, the true incidence and risk factors are presently unknown. More research is needed to determine a comprehensive list of risk factors and rumination disorder health risks.
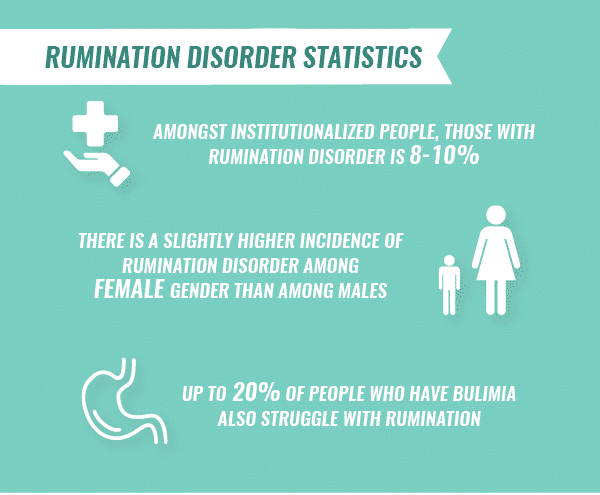
Rumination Disorder Statistics
Statistics on rumination disorder are difficult to find due to the lack of existing studies. Current rumination disorder statistics include:
- Amongst institutionalized people, the incidence of rumination disorder is8-10 percent
- There is a slightly higher incidence of rumination disorder amongfemale genderthan among males
- Up to20 percentof people who have bulimia also struggle with rumination
Rumination Disorder and Co-Occurring Conditions
Pica and rumination disorderare two separate conditions that may be associated with each other.Picais the eating of non-food or non-nutritive substances. While it may be possible that rumination occurs after pica, pica does not cause rumination.
Inone German study, the prevalence rates of recurring pica behavior were significantly elevated if recurring rumination disorder was present.
Related Topic:Treatment for pica
Additionally,bulimia and rumination disorder are two different conditions that people may think co-occur.Bulimiais a behavioral disorder that is the result of deliberate eating and purging with self-induced vomiting, use of laxatives or enemas. The purpose of these behaviors is to prevent weight gain in a person who has unrealistic body expectations. In contrast, rumination disorder is a medical condition that is involuntary regurgitation of food that is re-swallowed.
Rumination disorder and substance abusemay be related if the rumination is due to an underlyingdepressiveoranxiety disorderwhere the person self-medicates with alcohol or drugs. Substance abuse could also be associated with rumination directly because of the shame or embarrassment that the ruminator experiences.
Treatment for Rumination Disorder
Rumination disorder treatmentconsists of non-aversive and mild aversive techniques that are supportive and psychodynamic. If the rumination is to self-stimulate, the treatment results tend to be temporary. If it is socially motivated, then treatment can eliminate the symptoms. Some non-aversive techniques include:
- Small bites of food
- Chewing completely before swallowing
- Eating thick food
- Feeding techniques
- Habit reversal with relaxation
- Diaphragmatic breathing
- Hypnosis
- Biofeedback
- Guided imagery
- Weight reduction
- Addressing psychological issues or triggers
- Medications, if significant acid damage exists
If you or a loved one struggle with a drug or alcohol addiction and co-occurring rumination disorder, The Recovery Village can help. The Recovery Village facilities offer addiction treatment options as well as counseling for co-occurring mental health disorders.Reach out to a representativeto learn more.








