Obsessive-compulsive disorder (OCD) affects 2–3% of the population. Learning more about OCD statistics can reveal important information about this condition.
Obsessive-compulsive disorder is a mental health condition characterized by obsessive thoughts, compulsive behavior or a combination of both. The thoughts and urges to complete compulsive behaviors tend to be intrusive, unwanted, persistent and almost entirely out of the individual’s control.
Current obsessive-compulsive disorder statistics indicate that 1 in 40 adults in the U.S. have OCD. Reports show that OCD can affect children as young as five years old. Understanding OCD symptoms can help you identify if you or someone you know may suffer from this disorder, and OCD statistics demonstrate the prevalence of this condition.
Prevalence of OCD
OCD has gained attention in the media through TV shows or movies featuring characters with OCD. Much of the time the depictions are inaccurate or meant as a joke. Some may even use the phrase “Stop being so OCD!” when someone is especially particular or neat. Just how common is OCD in the general public, and who is affected by OCD?
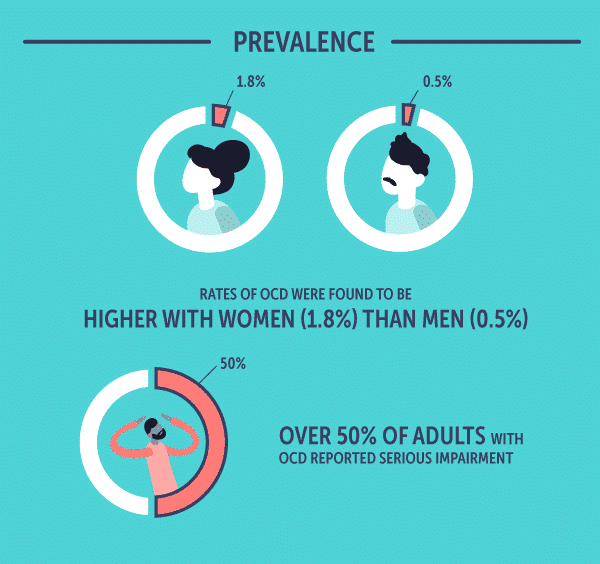
The National Institute of Mental Health provides an overview of the prevalence rate of OCD:
- For US adults aged 18 and up, 1.2% reported having OCD in any given year
- Rates of OCD were found to be higher with women (1.8%) than men (0.5%)
- The lifetime prevalence of OCD among U.S. adults was 2.3%
- Over 50% of adults with OCD reported serious impairment
Additional statistics on OCD prevalence include:
- Early-onset of OCD occurs most frequently with males, with one quarter being diagnosed before 10 years of age
- Most females are diagnosed after 10 years of age
- The average age of onset for OCD is 19.5 years
- Those diagnosed with OCD spend an average of nearly 9 years with the disorder
- 90% of people with OCD have another co-occurring disorder, such as anxiety or a mood disorder
- After the age of 30, new onsets of OCD are rare
Common OCD Obsessions
One of the core OCD symptoms is obsessions. OCD obsessions can be defined as persistent thoughts, impulses or images that are unwanted and often disturbing. Many times, these obsessive thoughts are accompanied by intense feelings of fear, disgust or doubt. The person with OCD may realize these thoughts are irrational, but they cannot control them. The persistence of these thoughts brings on anxiety and can severely affect one’s daily life.
Most common OCD obsessions involve:
Contamination
- Bodily fluids
- Germs
- Disease
- Contaminants
- Dirt
- Cleaning chemicals
Loss of Control
- Fear of violent or disturbing images in one’s mind
- Fear of the impulse to hurt oneself or others
- Fear of stealing
- Fear of blurting out expletives
Perfectionism
- Fear of losing or throwing out important items
- Need for exactness or evenness
- Need to remember, and fear of forgetting valuable information
Unwanted Sexual Thoughts
- Perverted thoughts concerning children or family members
- Forbidden sexual impulses or thoughts
- Obsessive thoughts about homosexuality
- Obsessive thoughts concerning aggressive sexual behavior toward another
Moral/Religious Concerns
- Excessive concern over moral right and wrong
- Excessive preoccupation with offending God
Harming
- Excessive fear of causing harm or damage to others
Hoarding
- Extreme attachment to old and useless possessions
- Intense anxiety to throw away items
Causes of OCD
Currently, there is no known definitive cause of OCD. While hereditary is thought to play a role, scientists are still not able to fully link OCD and genetics. Brain imaging studies have shown that the amygdala, the area of the brain known as the integration center for emotions and emotional behavior, could have an impact on the development of OCD.
Stress is a significant factor that may contribute to OCD. Stress can cause atrophy to certain parts of the brain and hypertrophy to other areas, including the amygdala. The symptoms from such stress are similar to OCD symptoms. Scientists are unsure if OCD is caused by trauma, or if extremely stressful, traumatic events trigger or exacerbate OCD symptoms.
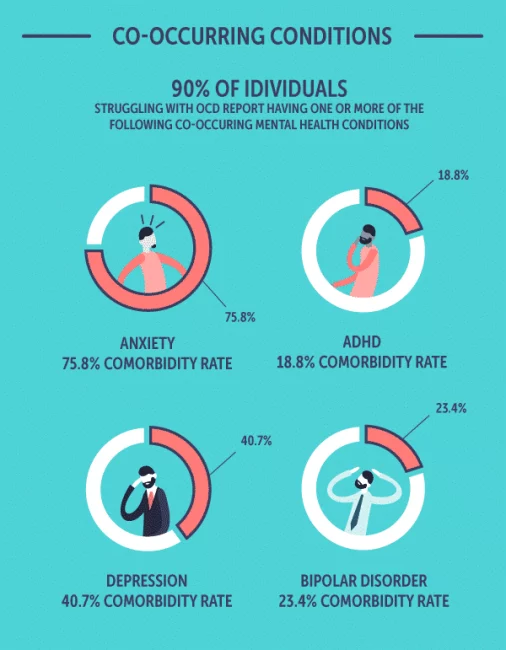
OCD and Co-occurring Conditions
OCD is commonly seen in combination with other mental health disorders. In a national survey, up to 90% of people with lifetime OCD had another existing mental health condition.
Some of the most common conditions that co-occur with OCD include:
- Anxiety: 75.8% comorbidity rate
- Attention-Deficit Hyperactivity Disorder: 18.8% comorbidity rate
- Depression: 40.7% comorbidity rate
- Bipolar Disorder: 23.4% comorbidity rate
Suicide is an important topic to discuss in relation to any mental health disorder. Historically speaking, OCD has been considered low for suicide risk. Recent studies have suggested otherwise. Certain factors can put someone with the condition at a higher risk of suicide, such as:
- Severity of OCD
- Severity of co-occurring disorders
- History of suicide attempts
- Range of unacceptable thoughts
- Feelings of hopelessness
The average rate of lifetime suicide attempts for people with OCD is 14.2%, while suicidal ideation rates can vary from 26.3–73.5%.
Diagnosing Obsessive-Compulsive Disorder
While most people may have occasional obsessive thoughts, these thoughts can usually be pushed out of the mind, and daily life and activities can continue as normal. This is not the case for people with OCD. The compulsions and obsessions characteristic of OCD are time-consuming and distressing to the point that they cause significant impairments in an individual’s personal and professional life.
An official OCD diagnosis can only be made by a mental health professional. Typically, a general health work-up with labs and blood tests is performed first to rule out any physical condition. If those tests come back clear, a thorough psychological examination is performed.
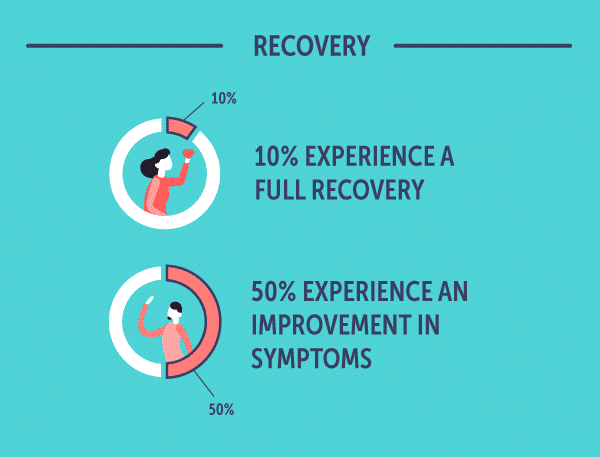
OCD Prognosis and Outlook
A speedy diagnosis is ideal, but one review estimated that it could take, on average, more than nine years to receive a correct diagnosis of OCD. Concerning OCD long-term prognosis, it can take an additional 17 years to receive adequate care. However, with proper treatment, 10% of people with OCD experience full recovery and 50% experience a marked improvement in symptoms.
For those with mild OCD symptoms or those who are averse to taking medicine, cognitive behavioral therapy (CBT) has been shown to help reduce symptoms. CBT focuses on equipping those who are experiencing symptoms with emotional and behavioral coping techniques.
Drug therapy has also helped many patients decrease the severity of their OCD symptoms. Often, the physician will start the OCD patient on an SSRI. The patient should expect about 10 to 12 weeks to elapse before they start noticing a change in symptoms.
Statistics on OCD Treatment and Recovery
In response to drug therapy, the OCD SSRI success rate can be as high as 40–60%. For those who stop taking SSRI’s, several studies have shown a high OCD relapse rate in symptoms. Some of these symptoms can be negated by gradually lowering the dosage of drugs taken while simultaneously engaging in CBT. One study showed the OCD relapse rate is lower in those who received CBT (20%) versus a limited course of drug therapy, which one study observed resulted in an OCD relapse rate of 90%.
If you or someone you know may be suffering from OCD and related substance abuse, please feel free to contact one of our representatives at The Recovery Village. Reach out today with for questions concerning our treatment program on our helpline, which is available 24 hours a day, seven days a week.


OCD Myths
Beyonocd.org. “Facts about Obsessive Compulsive Disorder.” 2019. Accessed April 19, 2019.
National Institute of Mental Health. “Obsessive-Compulsive Disorder OCD.” November 2017. Accessed April 19, 2019.
Landau, E. “OCD in Children: ‘A Darkness Has Overtaken Me.’” CNN Health, October 11, 2011. Accessed April 19, 2019.
Ruscio, A.M., et al. “The Epidemiology of Obsessive-Compulsive[…]y Survey Replication.” Molecular Psychiatry, January 2010. Accessed April 19, 2019.
Nestadt, G., Grados, M., Samuels, J.F. “Genetics of OCD.” Psychiatric Clinics of North America, March 1, 2011. Accessed April 19, 2019.
Ullrich, M., et al. “OCD-like behavior is caused by dysfuncti[…] SPREAD2 deficiency.” Molecular Psychiatry, February 2018. Accessed April 19, 2019.
Adams, T.G., et al. “The role of stress in the pathogenesis a[…]-compulsive disorder.” Chronic Stress (Thousand Oaks), March 4, 2018. Accessed April 19, 2019.
Albert, U. et al. “Suicide Risk in Obsessive-Compulsive Dis[…]a systematic review.” Current Neuropharmacology, June 20, 2108. Accessed April 19, 2019.
Harvard Health Publishing. “Treating Obsessive-Compulsive Disorder.” March 2009. Accessed April 19, 2019.
Feusner, J.D., et al. “Brain Connectivity and Prediction of Rel[…]-Compulsive Disorder.” Frontiers in Psychiatry, May 20, 2015. Accessed April 19, 2019.
Psiquiatr, R.B. “Full remission and relapse of obsessive […] two-year follow-up.” Brazilian Journal of Psychiatry, June 2010. Accessed April 19, 2019.
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.