Dysthymia may be more common than you think. Learn more about who it affects and how it can be treated through dysthymia statistics.
Depression is a fairly common condition that can impact one’s quality of life significantly. Not all depressive experiences are the same. Sometimes depression can be mild, but long-lasting. This is the case with dysthymia. Dysthymia is a type of depressive disorder that affects approximately 4% of the population. Pervasive depressive disorder is the term currently used to describe this condition in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders. Dysthymia facts and statistics reveal who is most commonly impacted by this condition, as well as what treatment options can improve their symptoms.
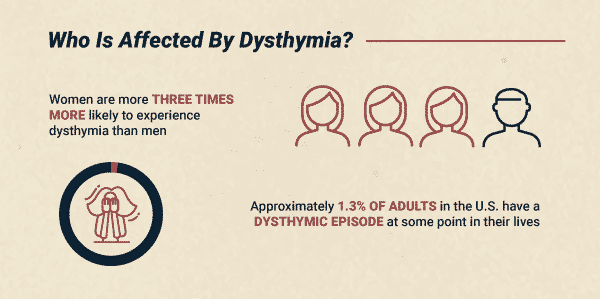
Who Is Affected By Dysthymia?
People of all ages, races, and genders can develop dysthymia. The condition is diagnosed in children after one year of symptoms. Dysthymia in adults is diagnosed after two years. Some other dysthymia facts include:
- Women are more three times more likely to experience dysthymia than men
- Approximately 1.3% of adults in the U.S. have a dysthymic episode at some point in their lives
- People with dysthymia diagnosis are more likely to have first-degree relatives with the condition
- Early onset of dysthymia (before age 21) is associated with an increased likelihood of having a personality disorder and substance use disorder
Age of Onset
The age of onset for dysthymia can vary. If someone is diagnosed before the age of 21, it is considered early-onset dysthymia. This condition is more likely to develop if someone experiences early trauma as a child, such as separation from a parent. People diagnosed after age 21 are considered to have late-onset dysthymia. If dysthymia criteria are met for two consecutive years, a co-occurring diagnosis of major depression should be given.
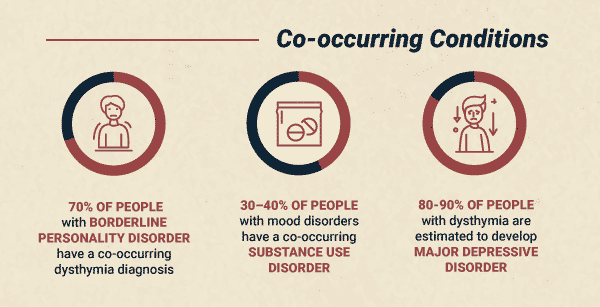
Rates of Dysthymia and Co-occurring Conditions
Dysthymia commonly coexists with additional diagnoses- most frequently with borderline personality disorder. People with borderline personality disorder have a co-occurring dysthymia diagnosis 70% of the time.
Dysthymia also frequently co-occurs with substance use disorder. Early experiences and genetic predisposition to dysthymia can make it more challenging to sustain emotional health, which can result in seeking external sources of stress reduction, like drugs and alcohol. Dysthymia and other mood disorders co-occur with substance use disorder 30–40% of the time.
Dysthymia and major depression tend to share many symptoms, though major depression is usually a more debilitating condition.
Diagnosing Dysthymia
Often people receive a dysthymia diagnosis after experiencing long periods of unremitting depressive symptoms. Dysthymia symptoms are similar to major depressive disorder but are less severe and longer in duration.
Some of the most common symptoms of dysthymia include:
- Feelings of sadness or hopelessness
- Sleep issues
- Appetite changes
- Tearfulness
- Low self-esteem
- Social withdrawal
- Guilt
- Lack of enjoyment
These symptoms are present for any age group diagnosed. Irritability can also be a factor for those with dysthymia, particularly children. These symptoms must be present for a minimum of two years — with the individual feeling down or depressed most days — for a dysthymia diagnosis to be made in adults. In children, a diagnosis can be made after one year of symptoms.
Statistics on Dysthymia Treatment
Dysthymia is a treatable condition. Dysthymia treatment success depends on an accurate assessment of the condition and treatment that involves therapy and antidepressant medications.
If you are struggling with co-occurring dysthymia and addiction and find yourself relying on the use of substances to cope, help is available. Reach out to take the first step toward healing. The Recovery Village can help you move toward health and wellness.


Healthresearchfunding.org. “18 Notable Dysthymia Statistics.” (n.d.) Accessed April 6, 2019.
National Institute of Mental Health. “Persistent Depressive DIsorder (Dysthymic Disorder).” November 2017. Accessed April 6, 2019.
Files.nc.gov. “Fact Sheet 5: Dysthymia.” 2008. Co-Occurring Disorders Program: Family Program. Accessed April 6, 2019.
Hurley, Katie, LCSW. “Persistent Depressive Disorder (Dysthymia).” Psycom.com, (n.d.) Accessed April 7, 2019.
National Education Alliance for Borderline Personality Disorder. “Making the Diagnosis.” (n.d.) Accessed April 7, 2019.
American Academy of Sleep Medicine. “Insomnia.” American Academy of Sleep Medicine, 2008. Accessed April 7, 2019.
Tartakovsky, M., “A Current Look at Chronic Depression.” October 5, 2018. PsychCentral.com. Accessed April 26, 2019.
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.