There are many different types of phobias that affect peoples’ daily lives. Learn about the most common phobias and phobia risk factors and treatment options.
Fear is a natural response to a real danger. A specific phobia, on the other hand, is an extreme fear of an object or situation that has little or no basis in reality.
While phobias might be triggered by real experiences — such as spider bites, airline disasters or elevator accidents — the fears eventually become disproportionate to reality. The distress associated with a phobia is so great that it can interfere with all aspects of a person’s life, including relationships, jobs, or social activities.
What Are Phobias?
By definition, a phobia is an irrational fear of an object, animal, situation or activity. This fear is unreasonable and unjustified but still doesn’t make it any less overwhelming for the person. People who have phobias will go out of their way to avoid the subject of their fear, even if it means restricting their lives to a self-destructive degree.
Phobias are also frequently associated with substance abuse. Drugs and alcohol may be used to soothe the intense reactions of a phobia or to calm the obsessive dread about encountering the object of fear.
Types of Phobias
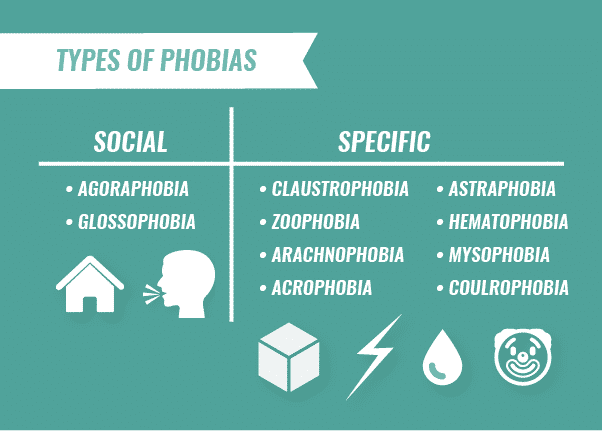
Although there are many different types of phobias, the two most common types include social phobias and specific phobias.
Social Phobias
Social phobias affect each person in different ways. Some people are frightened of specific situations, like being in crowded spaces with other people or speaking at a public meeting. For other people, social phobia symptoms may include a general, all-consuming dread of interacting with other people, regardless of what the situation may be.
- Agoraphobia. Agoraphobia is a fear of open spaces or social situations. People who have agoraphobia are so fearful of social situations that they isolate themselves in their homes, sometimes for months or years at a time. Panic disorder is common among people who have agoraphobia, as panic attacks can reinforce their dread of social situations.
- Glossophobia. Glossophobia, or the fear of public speaking, is one of the most common phobias. Even individuals who are self-assured and confident in other situations may be terrified of the idea of speaking in front of others. Glossophobia is especially debilitating for people who must speak before an audience or give public presentations as part of their professional lives, like politicians or teachers.
Specific Phobias
Specific phobias often co-occur with other disorders, such as generalized anxiety, obsessive-compulsive disorder or post-traumatic stress disorder. Specific phobias are irrational or unreasonable fears that are triggered by the presence of a specific object (or situation) that may pose no actual threat. For example, claustrophobia is a relatively common phobia about being trapped in an enclosed space. People who have claustrophobia usually fear small spaces, restricted movements and suffocation.
Other Common Phobias
There are a variety of common phobias. Some different types of phobias include:
- Zoophobia: fear of animals
- Arachnophobia: fear of spiders
- Acrophobia: fear of heights
- Aquaphobia: fear of specific situations, such as being in water
- Astraphobia: fear of natural phenomena, such as thunder and lightning
- Hematophobia: fear of blood or injuries
- Mysophobia: fear of experiences and objects like vomiting, choking, dirt and germs
- Coulrophobia: fear of clowns
- Nyctophobia: fear of dark places
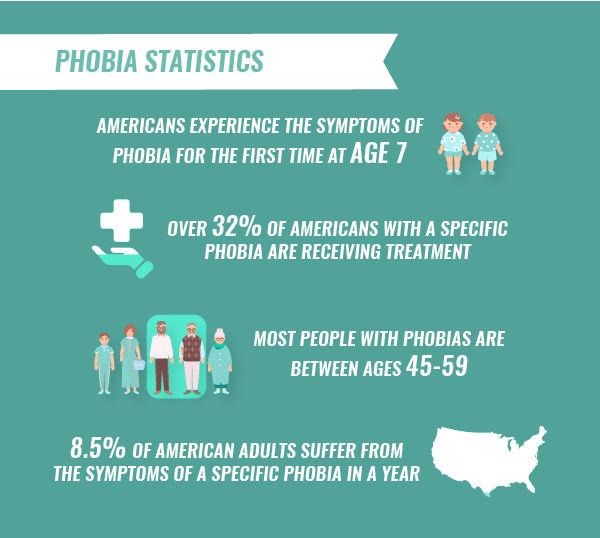
Phobia Statistics
Phobias affect a significant percentage of the American population. According to data from the National Institute of Mental Health, some phobia statistics include:
- Over 8.5 percent of American adults suffer from the symptoms of a specific phobia in any given year. Out of this group, the largest percentage is between the ages of 45 and 59.
- Over 32 percent of Americans with a specific phobia are receiving treatment for the disorder
- On average, Americans experience the symptoms of phobia for the first time at the age of seven
The Most Common Phobias
Out of the numerous phobias that have been identified, there are a few that prevail in our culture. According to Current Opinion in Psychiatry, the most common phobias involve animals, closed spaces, high places, being alone or being injured. However, although these top phobias occur the most frequently doesn’t mean that they are necessarily more debilitating than the more unusual phobias.
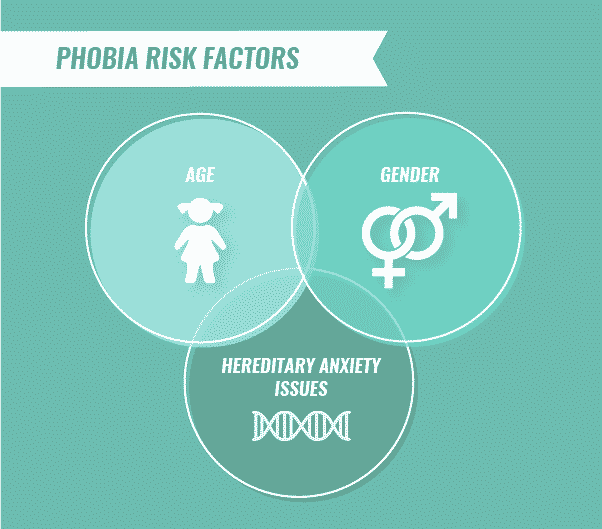
Phobia Risk Factors
Common risk factors of phobias include:
- Hereditary anxiety issues
- Age
- Gender
- Socioeconomic standing
Phobias and Substance Abuse
Like other anxiety disorders, specific phobias often co-occur with substance abuse. Alcohol and drugs may be used to take the edge off the individual’s persistent fears or to help him or her cope with depression caused by self-isolation. Substance abuse can temporarily mask the presence of a phobia. A neuropsychological evaluation is often required to distinguish between the symptoms of an anxiety disorder and the side effects of drug or alcohol abuse.
Diagnosing Phobias
Each type of phobia has its own unique set of diagnostic criteria. However, there are some overlaps. Diagnostic criteria that are similar for all phobias include:
- Life-limiting: the condition significantly impacts the person’s life
- Avoidance: extreme attempts to avoid the feared situation
- Anticipatory anxiety: tendency to dwell on upcoming events that may feature the feared object or situation
Phobia Treatment
Many effective therapies and phobia treatment options are available to help people. Several therapeutic strategies are successful, including:
- Cognitive behavioral therapy (CBT): Originally developed for the treatment of depression, CBT has been applied to the treatment of anxiety disorders and even phobias. This therapeutic approach aims to change the repetitive thought patterns that lead to self-defeating behaviors and distorted perceptions of the world. A person with a specific phobia, for instance, might learn to replace persistent worries about a situation or object with positive, reassuring self-talk.
- Exposure therapy: In exposure therapy, the patient is gradually exposed to the object of fear in a controlled environment. The ultimate goal is to introduce the patient to the subject of the phobia in a real-world setting. A person who is afraid of enclosed spaces (claustrophobia), for example, might set a goal of riding alone in an elevator without panicking. Exposure therapy must be performed at an appropriate pace to avoid overwhelming the patient.
- Psychiatric medications: Antidepressants in the SSRI (selective serotonin reuptake inhibitor) category have been used to treat specific phobias and other anxiety disorders. Benzodiazepine drugs may be prescribed on an as-needed basis for individuals whose anxiety attacks are limited to specific situations. However, because benzodiazepines have a high potential for dependence and abuse, their use must be carefully controlled.
- Relaxation techniques: Guided meditation, yoga, exercise therapy, music and art therapy, and massage therapy are a few of the relaxing practices that can help reduce stress and minimize anxiety symptoms in people with specific phobias.
If you or a loved one have a drug or alcohol addiction and a co-occurring phobia, The Recovery Village can help. To learn more about our dual diagnosis care, call The Recovery Village today and speak with a representative.


Swinson, R. “Social Phobia: a review in recent research trends.” Current Opinion in Psychiatry, March 2000. Accessed December 2018.
National Institute of Mental Health. “Specific Phobia.” Last updated 2017. Accessed March 2019.
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.