When left untreated, disorders like oppositional defiant disorder, intermittent explosive disorder and conduct disorder can dramatically impact a child’s physical and mental health.
When a child begins to act out, not follow rules or defy the directions of adults and authority figures, parents may wonder if their behavior is normal. They may also wonder what compels their loved one to engage in these unwanted behaviors.
All children have periods of disobedience, but for some, these behaviors cross the line from typical to pathological. A child who persistently ignores rules, threatens others or engages in violence and aggression could have a disruptive behavior disorder.
What Is Disruptive Behavior Disorder?
Disruptive behavior disorder (DBD) represents a group of mental health conditions with similar symptoms. Referred to as disruptive, impulse-control and conduct disorders by the American Psychiatric Association (APA), this group of conditions is noteworthy because they all involve violating the rights and desires of other people and create significant conflict with authority figures and unhealthy functioning in society.
Disruptive, impulse-control and conduct disorders affect an individual’s ability to control their emotions and behaviors. In many cases, this lack of control means that a person with one of these conditions may regularly injure others or break laws.
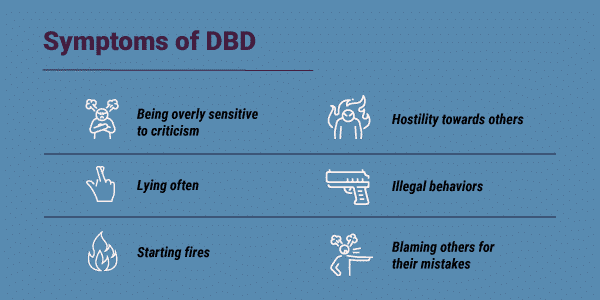
Symptoms of Disruptive Behavior Disorder
Although symptoms of disruptive behavior disorders vary based on the specific condition the person has, there are similar signs present in each diagnosis. Some common symptoms of disruptive behavior disorders include:
- Losing temper easily or being angered quickly
- Arguing with others frequently
- Refusing to do what is asked of them
- Annoying people intentionally
- Blaming others for their mistakes
- Being overly sensitive to criticism
- Feeling resentful or hostile towards others
- Hurting other people or destroying property
- Lying often
- Impulsively engaging in illegal behaviors, like stealing
- Starting fires
While many people engage in some of these behaviors at some point in their lives, those with a disruptive behavior disorder tend to exhibit these symptoms in ways that are:
- More frequent
- Longer in duration
- More intense
- More damaging
- Completed across different settings (not confined to home, school or work)
When a person has a disorder like depression, the person is usually the only one suffering the direct hardships of their condition. Family members will experience frustration and worry, but the condition only indirectly triggers these feelings. Disruptive behavior disorders differ from other mental health conditions because they cause the individual to take out their psychological distress in ways that negatively impact the outside world directly. For example, someone with a disruptive behavior disorder may hit, punch, kick, spit on, burn or verbally assault those around them, resulting in physical and emotional pain.
Types of Disruptive Behavior Disorder
There are three primary conditions in the group of disruptive, impulse-control and conduct disorders: oppositional defiant disorder, intermittent explosive disorder and conduct disorder. This group of disorders also includes less common conditions like pyromania, kleptomania and other specified disruptive, impulse-control and conduct disorder.

Oppositional Defiant Disorder (ODD)
A person with ODD does not listen to authority and instead follows their interests and wants. ODD affects a person in three ways:
- Mood problems: Individuals with this condition are usually annoyed, angry or resentful
- Defiance: Those affected by ODD frequently argue with authority, refuse requests, annoy others and blame other people for their mistakes
- Cruelty: People with this condition are often mean, spiteful or malicious to others
Instead of being isolated incidents, these feelings and behaviors are present consistently. Anyone can have ODD, but the first signs often present during the preschool years. ODD emerges after the early teens only in rare cases.
Intermittent Explosive Disorder
The second disruptive, impulse-control and conduct disorder listed by the APA is called intermittent explosive disorder. People with this condition are unable to control aggressive impulses, which they tend to have frequently. According to the APA, at any given time, about 2.7 percent of people in the U.S. have intermittent explosive disorder, with people under 40 comprising the majority.
A person with intermittent explosive disorder will display verbal aggression marked by:
- Temper tantrums
- Verbal arguments
- Fighting and bickering
These individuals also tend to exhibit physical aggression towards:
- Property
- Animals
- Other people
These behaviors must occur at least two times per week for three months for the individual to meet criteria for intermittent explosive disorder. The aggression displayed must also be out of proportion to the context for a diagnosis to be given. For example, someone with intermittent explosive disorder may severely injure a peer who bumped into them in the hall. It is also essential to note that these periods of aggression are never planned or premeditated. They are purely impulsive and driven by anger.
Conduct Disorder
The final common disruptive behavior disorder is called conduct disorder. Conduct disorder is a severe mental health condition that represents a consistent pattern of the individual hurting others and failing to fit in with normal social and societal behavior. In some cases, ODD is a precursor leading to conduct disorder. About 4 percent of people have conduct disorder, and the condition tends to be more common in men than women, according to the APA. Conduct disorder almost always begins by age 16.
A person with conduct disorder will engage in:
- Aggression toward others
- Destruction of property
- Lying and stealing
- Significant rule-breaking
People with conduct disorder tend to:
- Get suspended from school or fired from work
- Go to jail
- Have sexually transmitted diseases or unwanted pregnancies
- Smoke, drink and use drugs at early ages
- Show no guilt, shame or remorse for their actions
People with conduct disorder as children often grow up to be adults with antisocial personality disorder, a long-term condition characterized by frequent trouble with the law and inability to value other people.
Other Disruptive Behavior Disorders
Other disruptive, impulse-control and conduct disorders are less frequently found in the population, but can still produce a strong, adverse impact on the affected person’s life and the lives of others.
- Pyromania affects less than one percent of people in the United States. Symptoms include deliberate fire setting, tension, pleasure and arousal before, during and after fire setting and setting fires for no purpose other than a fascination with fire.
- Kleptomania is less common than pyromania and only affects about 0.5 percent of the population with women being three times more likely to have the condition, according to the APA. Symptoms of kleptomania include strong impulses to steal objects even when they are not valuable or needed, intense stress before the theft and intense relief and pleasure after the theft.
- An other specified or unspecified disruptive, impulse-control and conduct disorder diagnosis implies that a person has behavioral issues related to other disruptive behavior disorders, but their symptoms do not meet the full criteria for any of these conditions.
Related Topic: Pyromania treatment
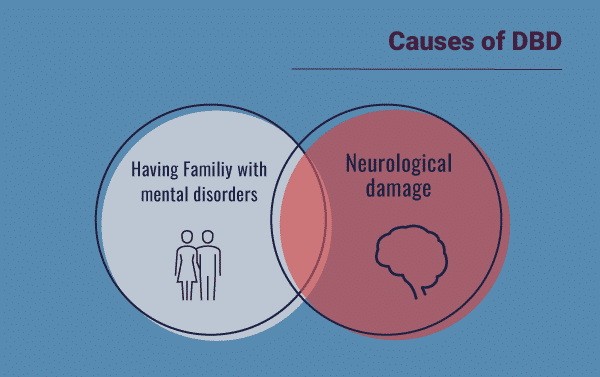
Causes of Disruptive Behavior Disorder
The group of conditions comprising disruptive, impulsive-control and conduct disorders are all influenced by a combination of biological and environmental factors.
Some biological factors that may influence the development of disruptive behavior disorders include:
- Low birth weight
- Neurological damage
- Having a family member with a similar disorder
- Having family members with attention-deficit hyperactivity disorder (ADHD), depression, bipolar disorder or schizophrenia
- Having parents who abuse alcohol and other drugs
- Having ADHD
There is some evidence that shows that people with disruptive behavior disorders display limited functioning in parts of the brain responsible for impulse-control and decision-making skills, which points to a significant influence of biological factors.
Environmental factors that can contribute to the emergence of disruptive behavior disorders include:
- Low income
- A history of abuse and neglect
- Being raised in homes with mothers who were abused
- Being rejected by their mothers as babies
- Being separated from parents and not provided supportive foster care
Diagnosing Disruptive Behavior Disorder
Two factors are crucial when making an accurate disruptive behavior disorder diagnosis:
- Determining if the person’s behavior is severe enough to distinguish it from normal acting out.
- Recognizing which disruptive, impulse-control or conduct disorder a person has. Identifying this can be difficult because ODD, conduct disorder and intermittent explosive disorder share many similarities.
Fortunately, experienced mental health professionals can usually access an individual’s symptoms and accurately diagnose the correct disorder. Professional diagnoses can be made by mental health professionals or primary care physicians.
Disruptive Behavior Disorder and Co-Occurring Conditions
The disruptive, impulse-control and conduct group of mental health disorders frequently occur with one or more other mental health conditions, referred to as co-occurring disorders. In some of these cases, individuals have more than one disruptive behavior disorder. Outside of this group, disruptive behavior disorders may co-occur with ADHD, anxiety disorders, depressive disorders and substance use disorders.
The presence of co-occurring conditions may complicate a person’s condition and worsen the impact on the individual’s life. In these cases, comprehensive treatment that addresses all disorders present is crucial to long-term mental and physical health.
Disruptive Behavior Disorder Treatment
Professional treatment for disruptive behavior disorders can help reduce symptoms and improve well-being. Experts recommend several styles of treatment for disruptive, impulse-control and conduct disorders involving the individual, their parents and their school.
- Family Therapy: By meeting with the client and the parents, a therapist can help parents understand how their reactions affect their child’s behaviors. Family therapy sessions focus on teaching new responses to parents while stressing the importance of consistency.
- Anger Management and Relaxation Skills: Since disruptive behavior disorders involve aggression and impulse-control problems, treatments focus on practicing anger management and relaxation. By tracking their anger, identifying the triggers of anger and completing helpful coping skills, patients with a disruptive behavior disorder can learn how to manage and work through difficult feelings and impulses.
- Classroom Interventions: A child with a disruptive behavior disorder needs consistency in all phases of life, and the classroom is no different. Teachers and other staff must set clear expectations for the student with meaningful reinforcements for desired behaviors and consequences for unwanted ones. This process can help guide the student towards more appropriate attitudes and behaviors.
- Medication: Psychiatrists have prescribed stimulant medications like Adderall and Concerta for years, but there is growing support to use the same group of medications for ODD and conduct disorder. When paired with therapy and other behavioral interventions, medications can help control symptoms.
Does My Child Need Help?
If you wonder about the role of a mental health condition in your child’s life and suspect that they may have a disruptive behavior disorder, it’s better to seek professional help sooner rather than later. As mentioned, many adolescents and young adults with a disruptive behavior disorder will also use alcohol and other drugs. Professional treatment is even more crucial if your child also grapples with addiction or other co-occurring mental health conditions.
If you believe someone you love has co-occurring substance use issues and disruptive behavior disorder, consider calling The Recovery Village. The Recovery Village is a treatment center specializing in dual diagnosis and co-occurring disorder with programs designed specifically for adolescents. Reach out to a representative today for more information.


American Psychiatric Association. “Diagnostic and Statistical Manual of Mental Disorders.” 2013.
CHADD. “Disruptive Behavior Disorders.” Accessed on March 23, 2019.
HealthyChildren.org. “Disruptive Behavior Disorders.” November 21, 2015. Accessed on March 23, 2019.
Parekh, Ranna. “What are Disruptive, Impulse-Control and Conduct Disorders?” American Psychiatric Association, January 2018. Accessed on March 23, 2019.
Substance Abuse and Mental Health Services Administration. “Characteristics and Needs of Children with Disruptive Behavior Disorders and Their Families.” 2011. Accessed on March 23, 2019.
Lumen. “Introduction to the disruptive behavior disorders.” Accessed March 26, 2019.
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.