Hypomania is an elevated mood state that may involve symptoms such as irritability, sleep disturbances, racing thoughts, risky behavior and elevated self-esteem.
Hypomania can occur in people with mental health issues. Though hypomania is less severe than mania, it can still cause unwanted symptoms and be detrimental to a person’s long-term mental health when left untreated. Learning more about the symptoms of hypomania can be the first step toward seeking help for this condition.
What Is Hypomania?
If you or a loved one is diagnosed with a mental health condition, you might be wondering, “What is hypomania?” A hypomania definition is as follows: an elevated mood state during which a person feels elated and can be overly active or productive. This mood state is typically associated with bipolar disorder.
While hypomania may sound appealing because of increased productivity, hypomanic episodes can become quite uncomfortable. People who are experiencing hypomania may be extremely irritable or engage in dangerous behaviors if symptoms are left untreated.
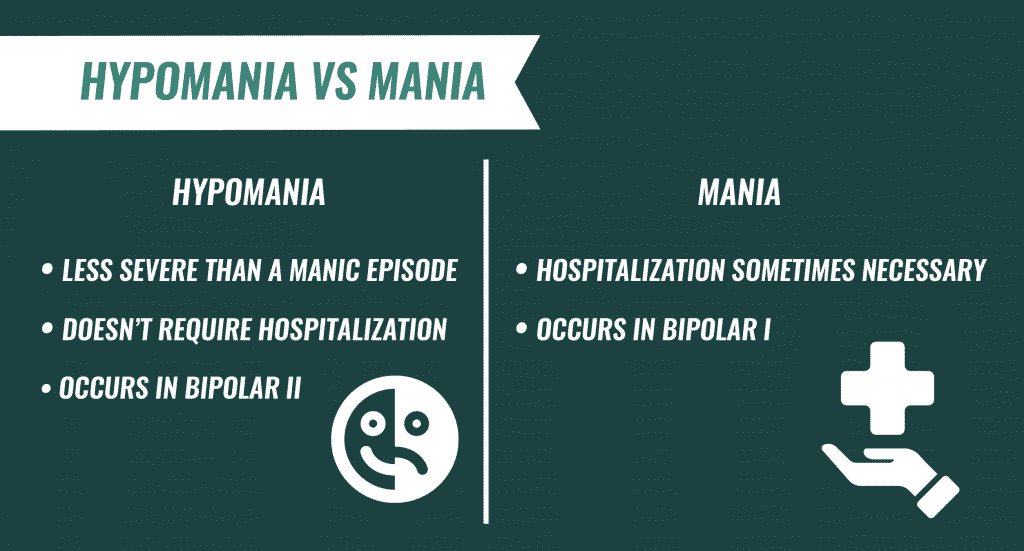
Hypomania vs. Mania
The difference between hypomania vs. mania is that a hypomanic episode is less severe than a manic episode. People who experience hypomania can typically be successful at school or work, and they do not display the psychotic features that can occur with full mania, according to the National Alliance on Mental Illness (NAMI). Hypomania also does not require hospitalization, which is sometimes necessary for mania. Another difference between hypomania and mania is that hypomania occurs with bipolar II disorder, whereas mania occurs in bipolar I.
Signs & Symptoms of Hypomania
Common hypomania symptoms provide information about what hypomania feels like. Symptoms can include:
- Heightened energy levels
- Irritable mood
- Unusually high self-esteem
- Delusions of grandiosity
- Talkativeness
- Sleep disturbances
- Racing thoughts
- Becoming easily distracted
- Risky behavior, such as gambling or unprotected sex
- Working toward many goals at once
- Fidgeting behaviors, such as pacing

How Long Does Hypomania Last?
The typical hypomania duration is four days or longer. The elevated mood seen during a hypomanic episode tends to be present the majority of the time on days when hypomania is occurring, according to diagnostic criteria.
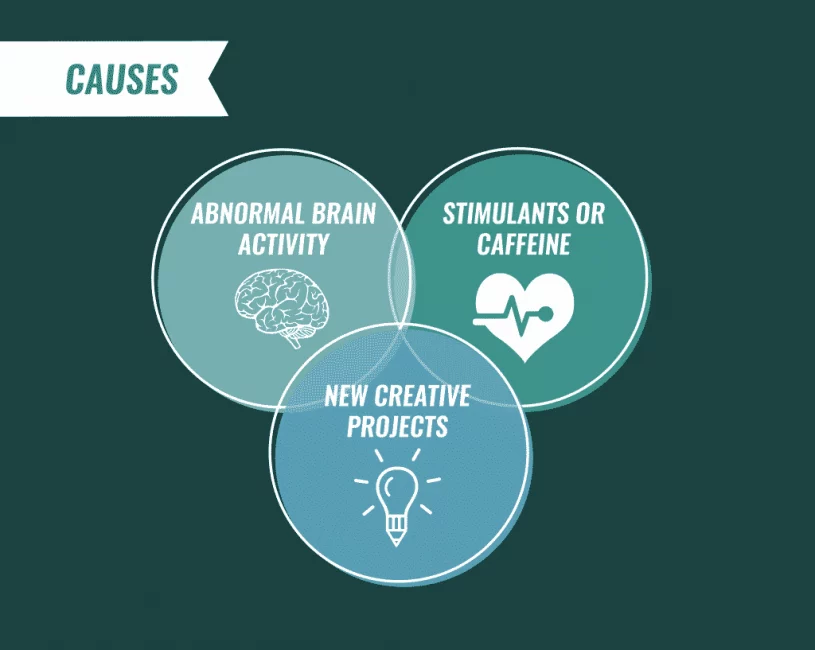
Causes of Hypomania
Hypomania result from abnormal brain activity that can occur in people with bipolar disorder. Certain factors can cause the onset of hypomania.
Hypomania triggers may include:
- Stimulant or caffeine use
- Late-night parties
- Loud music
- Taking on new creative projects
There is some evidence that disturbed sleep could be associated with the onset of bipolar disorder symptoms. Furthermore, a review of the research shows that circadian rhythm problems, life stressors, spring and summer weather, and personal factors, such as being emotionally expressive, are associated with an increased risk of experiencing hypomania and mania.
Diagnosing Hypomania
A mental health professional, such as a psychologist, psychiatrist, counselor or social worker takes on the role of diagnosing hypomania using criteria in the Diagnostic and Statistical Manual of Mental Disorders. During the diagnosis period, the clinician performs an assessment and discusses the individual’s mental health history and symptoms. With permission, the clinician may consult with a person’s family members or physician to gather additional information.
A diagnosis of hypomania occurs when a person has experienced an elevated or irritable mood state most of the time for at least four days. The person must also demonstrate between three or more of the symptoms associated with hypomania for diagnosis to be made.
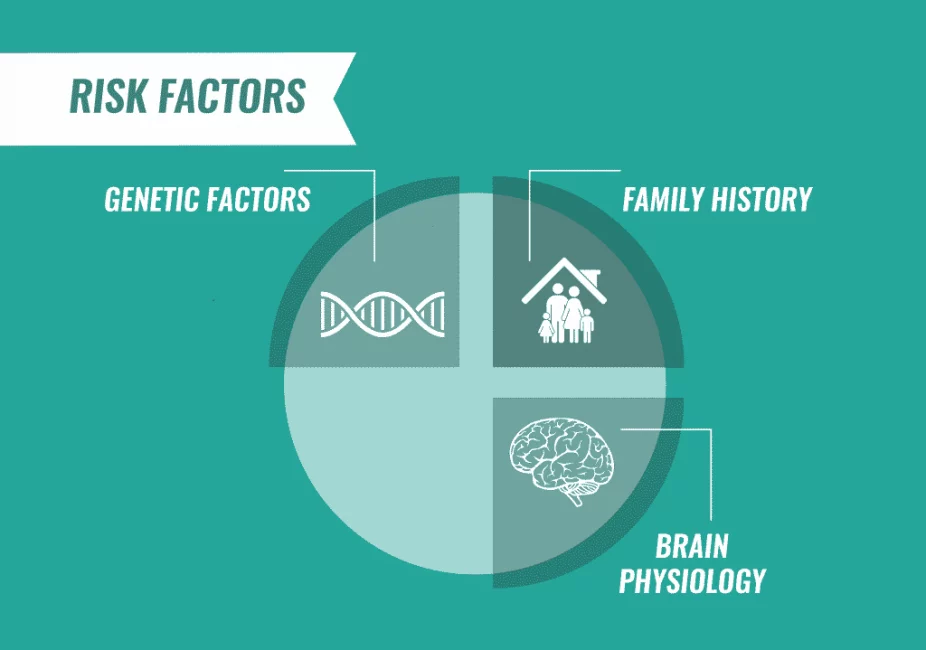
Who Is at Risk for Hypomania?
Certain people may be at increased of experiencing mood states like hypomania. Hypomania occurs with bipolar disorder, and the National Institute of Mental Health (NIMH) reports that risk factors for this condition include family history, genetic factors and differences in brain physiology. Hypomania risk factors tend to be the same factors that increase the risk of bipolar disorder.
Hypomania Statistics
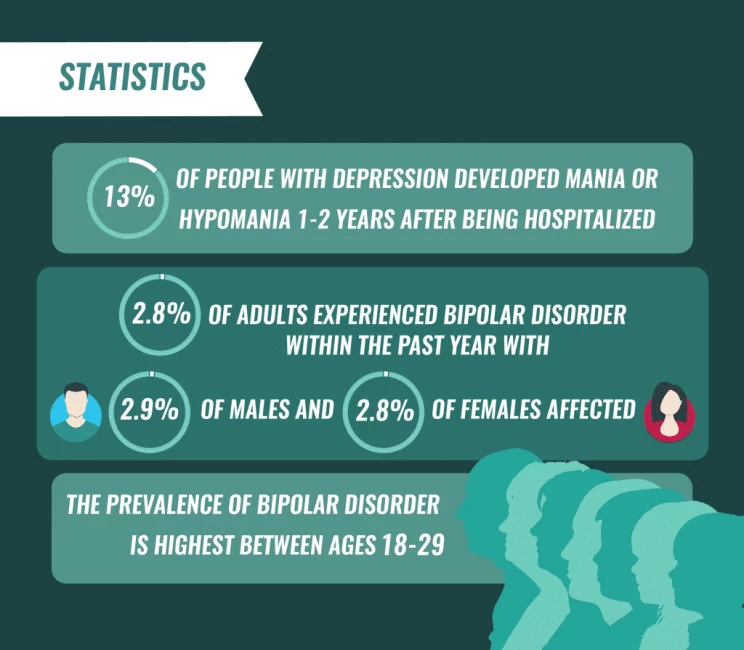
Hypomania statistics show that the risk of hypomania may be elevated in people who have been hospitalized for major depression, as one study found that 13 percent of people with depression developed mania or hypomania 1–2 years after being hospitalized for their condition. Other research suggests that people with inflammation may be at increased risk of developing hypomania.
Regardless of the specific causes of hypomania, men and women seem to be equally likely to experience this mood state. The NIMH reports that 2.8 percent of adults experienced bipolar disorder within the past year, with 2.9 percent of males and 2.8 percent of females being affected. The prevalence of bipolar disorder is highest between the ages of 18 and 29, at 4.7 percent. People in this age group may be more likely to develop hypomania.
Hypomania & Co-Occurring Disorders
In addition to bipolar hypomania, this mood state may co-occur with cyclothymia, a more mild form of bipolar disorder in which a person experiences some hypomania symptoms but does not meet full criteria for a hypomanic or depressive episode diagnosis.
Hypomania and substance abuse can also occur together. One study revealed that among people who experienced hypomania within the preceding year, 7 percent also experienced a drug use disorder and 24 percent had an alcohol use disorder.
The following conditions can co-occur with bipolar disorder and therefore may occur with hypomania:
- Anxiety disorders
- Eating disorders
- Attention-deficit hyperactivity disorder
- Thyroid conditions
- Heart disease
- Diabetes
- Obesity
Hypomania and depression can also co-occur, especially in cases of bipolar disorder in which a person experiences a mixed episode and demonstrates hypomania and depression concurrently.
Hypomania Treatment
Hypomania treatment typically involves a combination of medication and counseling. Someone who experiences hypomania may take mood-stabilizing medications like Lithium to normalize brain activity and prevent mood swings. Counseling services that teach coping mechanisms and techniques for identifying triggers can also provide some symptom relief. In addition, psychoeducation can help people learn how to calm hypomania.
If you or a loved one requires professional care for a co-occurring mental health condition and substance use disorder, The Recovery Village has locations around the country that provide comprehensive treatment services. Reach out to an admissions specialist today to take the first step toward recovery.
Related Topic: Treatment for mania


National Institute of Mental Health. “Bipolar disorder.”April 2016. Accessed April 4, 2019.
National Alliance on Mental Illness. “Bipolar disorder.” August 2017. Accessed April 4, 2019.
Substance Abuse and Mental Health Services Administration. “DSM-IV to DSM-5 hypomania criteria comparison.” June 2016. Accessed April 4, 2019.
Proudfoot, J., et al. “Triggers of Mania and Depression in Youn[…]ith Bipolar Disorder.” Journal of Affective Disorders, December 20, 2012. Accessed April 5, 2019.
Sylvia, L.G., et al. “Sleep Disturbance in Euthymic Bipolar Patients.” Journal of Psychopharmacology, August 2012. Accessed April 5, 2019.
Proudfoot, J., et al. “The precipitants of manic/hypomanic epis[…] of bipolar disorder.” Journal of Affective Disorders, October 2011. Accessed April 5, 2019.
DelBello, M.P., et al. “Rates and predictors of developing a man[…]h psychotic features.” Journal of Child and Adolescent Psychopharmacology, 2003. Accessed April 5, 2019.
Hayes, J.F., et al. “Childhood interleukin-6, C-reactive prot[…]l birth cohort study.” Psychological Medicine, January 2017. Accessed April 5, 2019.
National Institute of Mental Health. “Bipolar disorder: Definition.” November 2017. Accessed April 5, 2019.
Grant, B.F., et al. “Prevalence and co-occurrence of subst[…]d Related Conditions.” Archives of General Psychiatry, August 1, 2004. Accessed April 5, 2019.
National Institute of Mental Health. “Mental health medications.” October 2016. Accessed April 5, 2019.
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.