Depression is a mood disorder that causes a persistent feeling of sorrow and a loss of interest in everyday activities. It affects how an individual feels, thinks and behaves.
Many people have experienced a time in their life that brought them sadness and possibly caused them to lose interest in activities that they enjoyed before. Losing a loved one, relationship problems or getting fired from a job are all experiences that may cause sadness.
It is common for an individual to be sad and inactive temporarily after something disappoints them, though some individuals live with a crippling depression that does not go away. Depression is not just sadness. It is a mental illness.
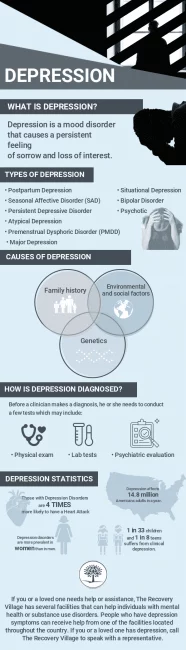
What Is Depression?
Depression is a mood disorder that causes a persistent feeling of sorrow and a loss of interest in everyday activities. Depression is most often called major depressive disorder or clinical depression in the mental health field. The disorder affects how an individual feels, thinks and behaves. It can also lead to a variety of emotional and physical problems.
Depression is more than just a case of the blues. Depression can keep individuals from completing daily tasks and can make them feel like life isn’t worth living. It is common to try to cheer up a sad friend, though depression isn’t a weakness. A person cannot just overcome the disorder. Depression may require long-term treatment.
Types of Depression
There are several different types of depression with varying symptoms, causes and severity. The following are some common forms of depression:
Major Depression
Major depression is a significant medical condition that can affect many areas of an individual’s life. It influences the patient’s mood, behavior and natural physical functions, such as appetite and sleep. Major depression may cause the individual to lose interest in activities that they enjoyed before and can create difficulties in performing everyday activities.
Persistent Depressive Disorder
Persistent depression, or dysthymia, is a less severe but more chronic form of depression. While this chronic depression is not disabling, it may still prevent a person from completing their daily routines. Even though this sadness is an extended depressed mood that lasts for two years or more, persistent depression is considered a mild form of depression.
Bipolar Disorder
Bipolar disorder, formerly called manic depression, causes extreme mood swings that might include emotional highs and lows. When an individual becomes depressed, they may feel sad or hopeless and lose interest in most activities. When their mood shifts to mania, they may feel overjoyed, full of energy or unusually irritable.
These mood swings can affect sleep, energy, activity, behavior and the ability to make a sound judgment. It’s sometimes difficult to distinguish between bipolar disorder and bipolar depression.
Seasonal Affective Disorder (SAD)
Seasonal depression relates to changes in seasons and reduced exposure to sunlight. The decreased amount of vitamin D from the sun links to this fairly common depression. Many individuals with SAD experience symptoms beginning in the fall and continue into the winter months. One can describe seasonal depression as a lack of energy and moodiness. Less often, SAD causes depression in the spring or early summer.
Psychotic Depression
Depression, or psychosis, that causes delusions or hallucinations is psychotic depression. Hallucinations could include hearing a voice telling the individual that they are not good enough or that they are worthless. Psychotic depression patients may experience delusions such as intense feelings of worthlessness or failure involving something that they are good at and other false realities.
Postpartum Depression
After giving birth, some mothers experience postpartum depression. This depression may occur during pregnancy or in the weeks or months after delivery.
Premenstrual Dysphoric Disorder (PMDD)
PMDD involves depression symptoms associated with hormone changes throughout the menstrual cycle. This depression is not just typical symptoms of premenstrual syndrome. In this form of depression, severe mood swings, anxiety and negative ideas surface in the week before the start of a woman’s period and dissolve once the menstrual period begins. Depressive symptoms are severe enough to affect relationships and interfere with daily functions negatively.
Situational Depression
Situational depression is a short-term, stress-related type of depression. It can develop after experiencing a traumatic event. Situational depression is considered an adjustment disorder. Adjusting to everyday life after a traumatic event can be challenging. Situational depression may be brought on by problems at work, school, illness, the death of a loved one, moving, relationship problems or other life-changing situations.
Atypical Depression
Atypical depression is a subtype of major depression that involves several specific symptoms, including increased appetite, ability to temporarily be cheered by happy events, excessive need for sleep, sensitivity to rejection and a heavy feeling in the arms or legs.
Symptoms of Depression
Depression is different from sadness, as it may completely consume a person in their day-to-day living. It continues for weeks, months and sometimes years and interferes with the individual’s work, school, relationships with other people and their ability to enjoy life. Some say depression feels like there is an empty hole inside them as they live life feeling hopelessness.
Most people who have depression do not necessarily experience every symptom of depression, and the presentation of the symptoms may vary in intensity from one individual to the next. Symptoms occur most of the day, nearly every day, and may include:
Physical signs of depression include:
- Loss of pleasure in normal activities, such as sex or hobbies
- Sleep disturbances
- Tiredness and lack of energy
- Reduced appetite or increased cravings
- Unexplained physical problems, such as pains or aches
Other symptoms include:
- Feelings of sadness, emptiness or hopelessness
- Slowed thinking, speaking or bodily movements
- Feelings of worthlessness, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering important details
- Angry outbursts, irritability or frustration, even over small matters
- Frequent or recurrent suicidal thoughts
Depression can cause problems in an individual’s everyday life, including relationships with others. It is common for those with depression to begin to care less about their productivity, getting to work on time, or showing up for events that they promised to attend. Depression can take over the individual’s mind and create bigger problems due to the symptoms.
Causes of Depression
Depression does not have a specific age, gender, race, career, relationship status or financial status that it attacks. It can affect anyone at any point in their life.
Like other mental disorders, researchers still can’t pinpoint what causes depression. Genetics, brain chemistry or neurobiological makeup, family history, personality, environment and social factors throughout development may all contribute to the disorder.
How is Depression Diagnosed
There are a few tests a general practitioner may conduct if an individual has symptoms of depression before making a depression diagnosis. However, many patients may need a referral to see a mental health professional for a psychiatric evaluation. Before a clinician makes a diagnosis, they typically conduct a few tests which may include:
- Physical exam: Practitioners may do a regular physical exam as well as ask questions about the patient’s health. Depression may link to an underlying physical health problem that an individual may be able to treat without psychiatric care.
- Lab tests: If the practitioner thinks it is necessary, they may conduct physical laboratory tests to obtain a blood count or test his or her thyroid to make sure it’s functioning properly. These tests will help rule out some other physical causes of the symptoms.
- Psychiatric evaluation: A mental health professional asks the patient about their symptoms, thoughts, feelings and behavior patterns. This evaluation may include filling out a questionnaire to help answer questions about feelings and behaviors.
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM5) outlines the following criteria to make a diagnosis of depression, which a clinician can discover through these psychological evaluations. The individual must be experiencing five or more symptoms on most days during the same two-week period. These symptoms typically include:
- Depressed mood most of the day
- Diminished interest or pleasure in all, or almost all, activities most of the time
- Significant weight loss or weight gain when not trying to change weight
- A slowing down of thoughts and physical movement or taking longer to complete tasks
- Fatigue or energy loss
- Diminished ability to think or concentrate or indecisiveness
- Feelings of worthlessness or excessive guilt
- Recurrent thoughts of death, suicidal ideation without a specific plan, a suicide attempt or a plan to commit suicide
These symptoms must cause the individual significant impairment in their social lives, work, school or other important areas of functioning to receive a diagnosis of depression.
Who Is at Risk For Depression
Depression often begins in the teens or early adulthood, but it can happen at any age. More women receive a diagnosis of depression than do men. This statistic may be due to the idea that women are more likely than men to seek treatment. Other factors include a personal or family history of other mental health disorders, such as anxiety disorder, suicide attempts, post-traumatic stress disorder or eating disorders.
Individuals have a greater risk of depression if they have experienced a serious or chronic illness, like cancer, stroke, chronic pain or heart disease. Other traumas can also be a contributing factor, such as stressful events that have occurred in the individual’s life.
These stressful events may include physical or sexual abuse, loss of a loved one, financial problems or a difficult relationship. If a person experiences anxiety, they are at high risk of developing depression.
A few other common risk factors for being diagnosed with depression include:
- Being uncertain of one’s sexuality or not being heterosexual
- Abuse of alcohol or illicit drugs
- Certain personality traits can lead to depression, such as being overly dependent, having low self-esteem and being self-critical or pessimistic
- Taking certain medications, such as some high blood pressure medications or sleeping pills
Depression Statistics
Adolescent depression is increasing at a high rate. Recent surveys conducted by the Center for Mental Health Services indicated that as many as 1 in 33 children and 1 in 8 teens deals with clinical depression.
Major depressive disorder affects approximately 14.8 million American adults or about 6.7 percent of the U.S. population in a given year. Depression disorders are more prevalent in women than in men.
Nearly half of the individuals who have anxiety also have depression. People with depression also face physical health risks. They are shown to be four times as likely as those without a history of depression to develop a heart attack. After a heart attack, people with depression are at an increased to experience a second heart attack or even death, according to the National Institute of Mental Health.
Depression Treatment
Common treatment options for depression include therapy and medication. Brain stimulation therapies such as Electroconvulsive therapy (ECT) and Repetitive transcranial magnetic stimulation (RTMs) may also be used in extreme cases. If someone struggles with co-occurring depression and substance abuse, treatment should address both conditions at the same time.
If you or a loved one needs help or assistance, The Recovery Village has several facilities that can help individuals receive treatment for depression and addiction. People who simultaneously experience drug or alcohol abuse and depression can receive help from one of the facilities located throughout the country.
If you or a loved one has depression and co-occurring substance abuse, call The Recovery Village to speak with a representative about treatment options.


The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.